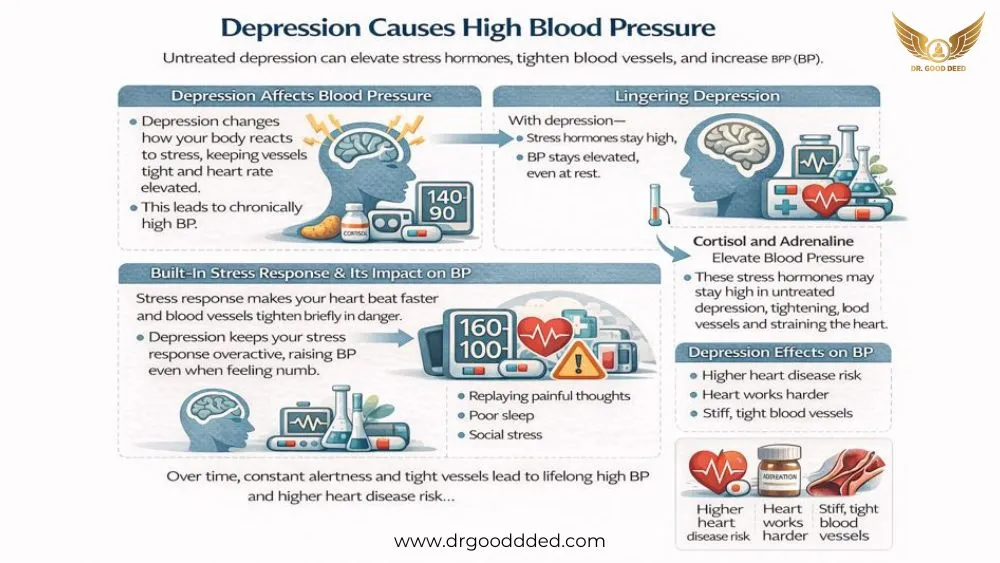
Depression can cause high blood pressure , especially when it stays untreated for long periods. Depression is a medical mood disorder that affects how you think, feel, sleep, and act, and it goes far beyond feeling sad for a few days. It changes brain chemistry and stress signaling, which directly affects your heart and blood vessels.
When depression lingers, your body releases more stress hormones like cortisol and adrenaline, keeping blood vessels tight and heart rate elevated. Over time, this constant “alert state” can push blood pressure higher, even at rest.
Depression also disrupts sleep, lowers physical activity, and increases unhealthy coping habits, all of which raise hypertension risk. People with long-term depression have a higher chance of developing chronic high blood pressure than those without depression.
How Depression Affects Blood Pressure
Depression changes more than mood. It changes how your body reacts to stress. Your heart and blood vessels respond to brain signals all day. When those signals stay tense, depression can cause high blood pressure in a real, physical way.
The Biological Stress Response And Its Impact On BP
Your body has a built-in alarm system. Doctors call it the stress response. It helps you act fast in danger. Your heart beats faster. Your blood vessels tighten. Your blood pressure rises for a short time.
Depression can keep this alarm system switched on. Even when you rest or feel “numb.” That constant alert state makes your blood pressure rise more often. Over weeks and months, this can add strain to your heart.
How Cortisol And Adrenaline Elevate Blood Pressure
Cortisol is a stress hormone. Adrenaline is another. When they rise, your blood vessels tighten. Your heart pumps harder. Your blood pressure climbs.
With depression, your body may release these chemicals more often. It can happen during rumination (replaying painful thoughts). It can happen after poor sleep. It can happen during social stress.
This is one reason depression can cause high blood pressure without you “feeling stressed.” Your body still runs stress signals in the background.
Chronic Emotional Stress And Long-Term Cardiovascular Strain
Short stress usually fades. Chronic stress keeps going. Depression often brings chronic stress. You may feel stuck in worry, guilt, or hopelessness. Your body reads that as a long threat.
Over time, tight blood vessels can lose flexibility. Your heart works harder to push blood through. That long strain matters for heart disease risk too. This supports the depression and heart health connection .
Can Mental Health Conditions Influence Blood Pressure?
Mental health can affect blood pressure . Mental health can shape your nervous system, hormones, and habits. Those three can shape blood pressure.
Depression and anxiety do not work the same way. But they can end at a similar result.
Anxiety Vs Depression: Different Pathways, Similar BP Effects
Anxiety often causes sudden surges. Your heart races. Your breathing speeds up. Your blood pressure jumps.
Depression often causes longer wear. You may move less. You may sleep poorly. You may feel constant internal pressure. That can lead to steadier blood pressure strain.
Both paths can raise risk over time. That is why many people notice that anxiety and depression can cause high BP patterns in the same year.
The Role Of Rumination And Chronic Worry
Rumination means your mind replays the same painful thought loop. Chronic worry keeps you scanning for problems. Even when nothing is happening.
That looping can trigger stress hormones again and again. It also makes sleep harder to sleep. If you keep waking at night, your blood pressure may stay higher the next day.
Rumination also changes your body’s “reset” system. Your heart may not slow down as well after stress. Researchers study this using heart rate variability (HRV). Lower HRV is often linked with depression and stress.
How Mood Disorders Disrupt Heart–Brain Communication
Your brain and heart talk through nerves and chemicals. A key system is the autonomic nervous system. It has two main parts. One part speeds you up. One part calms you down.
Depression can tilt this balance. You may get fewer “calm” signals and more “go” signals. Studies link depression with autonomic changes and HRV differences. When that happens, depression can cause high blood pressure more easily during daily stress.
Emotional Stress And High Blood Pressure
Stress does not always cause long-term hypertension. But it can cause spikes. Those spikes can add up. In many people, emotional stress increases high blood pressure in the moment. If the pattern repeats often, your baseline readings may creep up.
Acute Spikes Vs Chronic Hypertension
Acute spikes are short. They happen during an argument. They happen during a scary email. They happen during a panic wave. Your pressure rises, then drops.
Chronic hypertension means the numbers stay high across many readings. It often has no obvious symptoms. That is why it can hide for years.
Depression can fit both. It can raise spikes through stress signals. It can support chronic patterns through sleep loss and lifestyle shifts. This is another way depression can cause high blood pressure .
Stress-Induced Behaviors That Worsen BP (Smoking, Alcohol, Overeating)
Depression can push you toward quick relief. That relief often comes with a cost.
Nicotine can tighten blood vessels fast. Alcohol can raise blood pressure in many people, especially with regular use. Comfort eating often means more salt and more ultra-processed food. Extra salt can raise blood pressure in salt-sensitive people.
These behaviors also make stress recovery harder. When you feel worse, you may cope harder. That loop can raise pressure again. Over time, depression can cause high blood pressure through habit pathways, not just hormones.
How Sleep Disturbances From Depression Raise BP
Sleep problems are common in depression. You may wake early. You may wake many times. You may sleep too long but still feel tired.
Poor sleep keeps your stress system active. It also reduces the normal nighttime dip in blood pressure. If your body does not dip at night, your heart gets less rest.
So if you feel depressed and sleep breaks down, you may see higher morning readings. That does not prove a diagnosis by itself. But it is a strong clue.
Depression, Anxiety, And Their Combined Effect On Hypertension
Depression and anxiety often show up together. When they do, blood pressure issues can feel stronger. This is not about weakness. It is about body wiring.
Why Co-Occurring Anxiety Increases BP Risk More Than Depression Alone
Anxiety adds frequent spikes. Depression adds long-term recovery problems. Together, they can keep your body revved up and slow to calm down.
That is one reason clinicians take the combo seriously. It also explains why anxiety and depression can cause high BP more often than depression alone.
Autonomic Nervous System Dysregulation
Dysregulation means the system does not adjust smoothly. Your heart rate may stay high longer after stress. Your vessels may stay tight longer, too.
Researchers often use HRV as a window into this. Many reviews report HRV changes across mental disorders, including depression and anxiety. This matters because autonomic balance helps control blood pressure during normal life.
Physical Symptoms Of Emotional Distress That Influence BP
Emotional distress can show up as bodily symptoms. You may feel chest tightness. You may feel headaches. You may feel stomach pain. You may feel dizzy and constant fatigue.
These symptoms can scare you. Fear can raise pressure. The symptoms can also reduce activity. Less movement can raise blood pressure over time. This is another path where depression can cause high blood pressure .
Depression And Heart Health:
Depression does not only affect feelings. It relates to heart outcomes in research. Reviews describe links between depression and worse cardiovascular outcomes. Public health research also tracks depression alongside heart risk markers. This supports the depression and heart health connection as a real medical concern.
Evidence Linking Depression To Hypertension Risk
A well-cited meta-analysis of prospective studies found depression likely raises the risk of developing hypertension. Newer meta-analyses also report a significant association between depression and hypertension risk. These findings cannot prove a direct cause in every person. Lifestyle, genes, and other illnesses can play roles too.
Still, the pattern shows up often enough that clinicians treat depression as a meaningful risk factor. This is the research backbone behind the depression and hypertension risk .
Increased Inflammation And Cardiovascular Strain
Inflammation means your immune system stays activated. Some studies link depression with higher inflammation markers. Inflammation can affect blood vessel function over time.
Stiffer vessels can raise blood pressure. A stressed heart can struggle more during daily tasks.
This does not mean inflammation explains everything. But it adds one more route where depression can cause high blood pressure .
Why Untreated Depression Increases Long-Term Heart Disease Risk
Untreated depression can last for years. Years matter. Long depression can mean long poor sleep, low movement, and higher substance use. It can also mean missed medical care.
Research links depression with higher heart disease risk and worse outcomes in people with heart disease. So the goal is not only “feel better.” The goal is also to protect your long-term health.
When you stay untreated, depression can cause high blood pressure more easily over time and with repetition.
Can Antidepressants Affect Blood Pressure?
Sometimes, yes. It depends on the medicine, your dose, and your body. This matters because depression can cause high blood pressure , and a few antidepressants can also nudge blood pressure upward in certain people.
Medications That May Raise BP (SNRIs, Certain Stimulants)
SNRIs (serotonin-norepinephrine reuptake inhibitors) affect norepinephrine (a stress chemical). That change can tighten blood vessels and raise BP in some patients. The FDA label for duloxetine notes that blood pressure should be checked before starting and during treatment, and it reports average BP increases at higher doses.
Venlafaxine is another SNRI that can raise BP, and rare cases of severe BP elevation have been reported, including hypertensive crisis in case reports.
Stimulants can raise BP too, especially if they increase heart rate and “fight-or-flight” signals. If you have already noticed that emotional stress increases high blood pressure , stimulants can sometimes amplify that pattern in sensitive people.
Antidepressants That Typically Do NOT Raise BP
Many SSRIs (like sertraline, fluoxetine, and citalopram) usually have a limited impact on blood pressure for most people. A major review in cardiovascular medicine describes SSRIs as having a lower BP impact compared with other antidepressant classes.
Here is a quick view that helps you skim:
| Medicine Type | BP Pattern Seen In Research | What You Do |
| SSRIs | Usually minimal BP change | Still check BP if you have hypertension |
| SNRIs | Can raise BP in some people | Monitor BP more closely |
| Stimulants | Can raise BP and pulse | Ask about safer options if BP climbs |
When To Talk To Your Doctor About Medication-Related BP Changes
Talk to your clinician if your home readings rise and stay high for more than a few days after a new medicine or dose change. Also, talk if you get strong headaches, chest pressure, or racing heartbeat. Do not stop antidepressants suddenly. Dosage varies by age and condition, and stopping too fast can cause withdrawal symptoms.
Lifestyle Factors Connecting Depression And High BP
Even if you do everything “right,” depression can cause high blood pressure through biology. But lifestyle can still push your numbers up or down. Depression often changes lifestyle in ways you do not notice at first.
Sedentary Behavior And Reduced Physical Activity
When depression hits, you move less. That is not laziness. Your brain’s reward and energy systems slow down. Less movement can lead to weight gain, worse sleep, and higher resting BP over time.
If you also have anxiety, the body can swing between tension and shutdown, which is one reason anxiety and depression can cause high BP patterns that feel confusing.
Poor Diet, Emotional Eating, And Weight Gain
Depression can change appetite. You may crave salty snacks or sweet foods because they give quick comfort. High-salt foods can raise BP in salt-sensitive people. Weight gain can also raise BP by increasing strain on blood vessels. This is a common bridge between depression and hypertension risk .
Alcohol, Nicotine, And BP Spikes
Alcohol can raise BP for many people, especially with regular intake. Nicotine can spike BP fast by tightening blood vessels. If emotional stress increases high blood pressure for you, alcohol and nicotine can make the spikes sharper and recovery slower.
Diagnosing High Blood Pressure In People With Depression
Diagnosis sounds simple, but real life gets messy. Depression can hide symptoms, reduce checkups, and make you doubt your own signals. That is how depression can cause high blood pressure to go unnoticed until a routine reading catches it.
Why Symptoms May Go Unnoticed
High blood pressure often has no clear symptoms. You might feel fine. Depression can also make you ignore body cues. You may assume fatigue comes from mood, not from poor sleep or high BP.
Home Blood Pressure Monitoring During Stress
Home monitoring helps because it shows patterns. If possible, check at the same times each day, and write down sleep quality, caffeine, and stressful events. If your BP jumps mainly on high-stress days, that supports the idea that mental health can affect blood pressure in your case.
Also watch for “white coat” effects. Some people spike in clinics due to nerves. Home readings can give a calmer baseline.
How Clinicians Evaluate Mental Health And BP Together
A good clinician looks at both tracks. They may screen for depression and anxiety, ask about sleep and alcohol, and review medicines. This matters because the depression and heart health is not only about feelings. It is also about long-term vessel strain and heart risk seen in research.
Treatment Strategies For Managing Both Depression And High BP
Treating one condition often helps the other. When your mood improves, you usually sleep better and move more. When BP improves, you often feel less physical stress. That two-way benefit can weaken the cycle where depression can cause high blood pressure .
Therapy Approaches (CBT, Mindfulness, Stress-Management)
CBT (cognitive behavioral therapy) helps you spot thought traps and change your response. That can reduce rumination and stress surges. Mindfulness teaches your body to downshift from “alert” mode. Stress-management skills help you recover faster after triggers, which matters if emotional stress increases your high blood pressure .
Lifestyle Interventions That Improve BP And Mood
You do not need huge changes. You need repeatable ones. Regular walking, steady sleep timing, and simple meals can support both mood and BP. If you also have anxiety symptoms, these routines reduce the physical arousal that explains why anxiety and depression can cause high BP for some people.
When Medication And Therapy Should Be Combined
Some depression is too heavy for skills alone at first. Combined care can help you stabilize. If you have hypertension, your clinician can choose options with fewer BP effects and monitor you. This approach respects the depression-hypertension risk without creating fear around treatment.
Prevention: Lowering Your BP While Managing Depression
Prevention is not perfection. It is reducing repetitive stress and building recovery into your day. That matters because depression can cause high blood pressure through repeated body strain.
Stress-Reduction Techniques That Reliably Lower BP
Slow breathing can calm the nervous system. A short walk after stress can lower tension. Short “reset” breaks can stop stress from stacking all day. These tools help because mental health can affect blood pressure through nerve signals, not just thoughts.
Heart-Healthy Habits That Also Improve Mood
Lowering alcohol, reducing nicotine, and improving sleep can help both mood and BP. Regular movement supports vessel health and lowers stress chemistry. These habits strengthen the depression and heart health connection in the right direction.
Building A Long-Term Wellness Routine
Choose routines you can do on your worst day. Make them small. A five-minute walk counts. A set bedtime counts. A simple breakfast counts. Small habits reduce the daily load that fuels emotional stress and increases high blood pressure .
When To Seek Medical Help
You should not “wait it out” if your numbers are dangerously high or your depression becomes unsafe.
Warning Signs Of Dangerously High Blood Pressure
If your blood pressure is higher than 180/120 and you have symptoms like chest pain, shortness of breath, weakness, vision changes, or trouble speaking, it is an emergency. Call emergency services.
When Depression Becomes A Medical Emergency
If you think about self-harm, feel unable to stay safe, or cannot control dangerous impulses, get urgent help right away. You deserve fast support, not judgment.
Questions To Ask Your Doctor
Ask if your BP pattern looks stress-related or chronic. Ask how often to monitor at home. Ask if any medicines could raise BP. Ask how to treat both conditions together, especially if depression causing high blood pressure has become a real worry for you.
FAQs
Can Depression Directly Cause Long-Term High Blood Pressure?
Yes, sometimes. Research suggests a real link, but not everyone develops hypertension. Your risk rises through stress hormones, sleep disruption, and lifestyle shifts. Depression can cause high blood pressure most often when stress remains chronic.
Does Emotional Stress Make Your Blood Pressure Spike Temporarily?
Yes. Short stress can raise BP for minutes or hours. If spikes happen often, your baseline can creep upward. That is why doctors take patterns seriously when emotional stress increases high blood pressure for you.
How Does Anxiety Combined With Depression Affect BP Levels?
The combo can cause more stress surges plus weaker recovery. Anxiety drives spikes, and depression weakens sleep and activity. That overlap explains why anxiety and depression can cause high BP in real daily life.
Which Antidepressants Can Raise Blood Pressure?
Some SNRIs, like duloxetine and venlafaxine, can raise BP in some patients. Labels and reviews advise monitoring, especially after starting or changing doses.
Can Treating Depression Lower High Blood Pressure Naturally?
It can help. Better sleep, less alcohol, more movement, and fewer stress surges can reduce BP over time. Treating mood can break the cycle where depression can cause high blood pressure through daily strain.
Is High Blood Pressure From Stress Dangerous?
A single spike can be risky if it reaches crisis levels. Repeated spikes add wear on vessels over time. If your reading is 180/120 or higher with symptoms, treat it as an emergency.
How Can You Tell If Stress Or Depression Is Affecting Your BP Readings?
Track readings at consistent times and note sleep, caffeine, conflict, and panic symptoms. If the pattern matches your mood swings, it supports that mental health can affect blood pressure for you, and you should discuss it.
Can Lifestyle Changes Improve Both Depression And High BP?
Yes. Regular movement, steady sleep timing, and lower alcohol and nicotine use can help both. These changes reduce depression and hypertension risk and also reduce stress spikes linked to mood symptoms.
Does Chronic Stress Increase Heart Disease Risk?
Chronic stress keeps vessels tight and hormones high. Over time, this can raise BP and harm heart health. That is part of the depression and heart health connection doctors take seriously in long-term care.
When Should You See A Doctor For BP Changes Related To Depression?
See a doctor if your readings stay high across multiple days or if a new medicine changes your BP. Seek emergency care for 180/120 with symptoms. Depression can cause high blood pressure , but you should not self-diagnose without measurements and medical review.












Leave a Comment