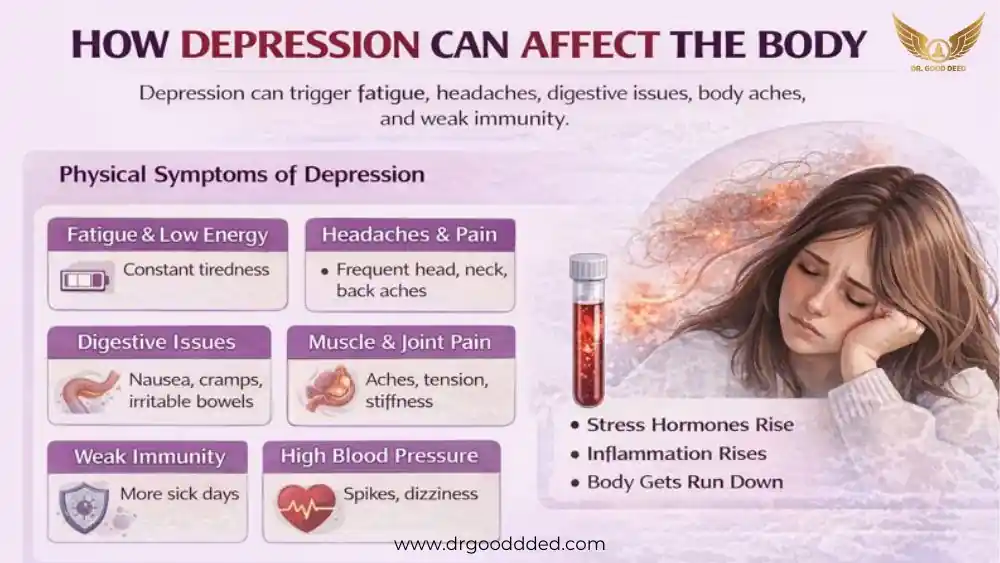
Depression is a medical condition that affects the way you think, feel, and function, and it can also create real physical changes throughout your body. It is more than sadness because it disrupts brain chemicals that guide sleep, appetite, pain control, energy, and the stress response.
When these systems shift, depression can make you sick by triggering fatigue, headaches, muscle pain, stomach trouble, weak immunity, and high blood pressure spikes. Your body stays in a stress state for long periods, which raises inflammation and lowers your ability to recover from normal daily strain.
This is why people with untreated depression often notice more aches, slower healing, and frequent digestive issues even when no infection or injury is present.
Physical Symptoms of Depression
When you have a low mood, your body often reacts. You may notice changes in sleep, appetite, energy, and pain. These signs are common, and they can be serious. Immune signals and inflammation often rise in people with depression. This may help explain why depression can make you sick .
How Chronic Stress Disrupts the Immune System
When you feel stressed for weeks or months, your stress hormones stay high. Cortisol and related hormones alter the function of white blood cells. Over time, your immune response can weaken or become more inflammatory. That means you get sick more often and take longer to heal.
Long-term stress and depression lead to higher inflammatory markers in blood. The research is strong that stress and some types of depression raise inflammation, but the exact size and timing of the effect still need more study.
Why Depression Causes Fatigue and Low Energy
You may rest and still feel exhausted. Depression changes brain circuits that drive motivation. Hormones and sleep also change. Low dopamine and shifts in serotonin and norepinephrine can lower your drive and energy.
In some people, fatigue relates to inflammation and immune activity. This makes exercise feel harder even when it would help. The pattern is common, though the exact pathways vary between people.
The Link Between Depression and Headaches or Migraines
If you have tension and low mood, head pain often rises. Muscle tightness in the neck and shoulders adds strain. People with depression get more frequent headaches and worse migraines.
Pain and mood share brain pathways. Treating mood can lower headache frequency for some patients. Some trials show benefit, but not all patients respond the same way.
Digestive Symptoms: Nausea, Stomach Discomfort, and IBS-Like Issues
The gut and brain talk to each other constantly. Stress alters gut movement, gut sensitivity, and gut bacteria. You may get nausea, cramps, bloating, or bowel changes. These are often labeled as IBS-like signs (IBS means irritable bowel syndrome).
Treatments that reduce stress and improve mood often ease gut symptoms. Still, gut findings are mixed across studies, and more targeted trials are needed.
Muscle Aches, Back Pain, and Joint Stiffness from Stress Hormones
Stress makes muscles stay tight. Over days, tight muscles develop trigger points and pain. Inflammation can add deeper aches. You often have neck, back, or shoulder pain when your mood is low. This is partly why depression can make you sick with aches that feel like physical injury, even when scans look normal.
Sleep Disturbances That Worsen Physical Illness
Poor sleep harms repair and raises pain. You may fall asleep slowly, wake often, or sleep too much. Bad sleep raises inflammation and harms glucose control. When sleep stays poor, you recover more slowly from infections and injuries.
Fixing sleep often reduces other physical symptoms. Sleep changes are a key physical sign linked to mood disorders. Improving sleep helps both mood and body, though the best sleep approach varies by person.
Can Depression Cause Body Pain?
How Serotonin And Norepinephrine Imbalance Increases Pain Sensitivity
When serotonin and norepinephrine drop, the pain-control pathways in your brain and spinal cord become less effective. These chemicals help your nerves filter pain, so when they fall, your body reacts more strongly to aches that would normally feel mild.
This is one reason depression can make you sick , because the same physical trigger suddenly feels sharper and harder to ignore, even when nothing severe has changed in your tissues. People dealing with low mood often notice that headaches, muscle soreness, or back pain grow worse during emotional stress.
Some antidepressants ease pain because they raise these chemicals, but results differ between people. Doctors study these shifts closely because not everyone has the same chemical pattern, and the science still needs more precise testing.
Why Inflammation Rises During Depression
Chronic emotional strain activates your immune system in subtle ways. In many studies, people with depression show higher levels of inflammatory markers such as CRP or certain cytokines.
These signals make your nerves react more strongly to pain and raise soreness across the body. This inflammatory shift helps explain how depression can make you sick even when there is no infection. It also helps explain why body pain and fatigue often appear at the same time as mood symptoms.
Some people show strong inflammation during depression, while others show little change.
Chronic Tension’s Impact on the Neck, Shoulders, and Spine
When emotional stress builds, your muscles stay tight for long periods, especially in the neck, shoulders, and spine. This tension reduces blood flow to the muscles and creates stiff knots known as trigger points. These knots make everyday movement painful and cause soreness that spreads into your head or back.
Over time, tension becomes a habit, and you may not notice how often you clench your jaw, raise your shoulders, or hold a stressed posture. This pattern contributes to why depression can make you sick and physically strained.
Doctors and therapists see this often in people with anxiety and depression. Treatment usually focuses on releasing tension while improving mood. Light stretching, heat, posture changes, and physical therapy can help reduce knots.
Pain Amplification in Long-Term Depression
Long-term depression can change how your nervous system reads pain signals. When the brain stays in a stressed state, it becomes more alert to pain, even when the cause is small. The same pressure that once felt mild may feel intense.
This process, known as central sensitization, helps explain why depression can make you sick with pain that spreads across the body without a clear injury. People often describe pain moving from one area to another, which confuses them and delays treatment.
This shift is reversible with the right care. When mood improves, brain pathways calm down and pain often becomes more manageable. Still, this process takes time, because the nervous system adapts slowly.
How Depression Affects the Body Beyond Mood
Cardiovascular Changes: Increased Heart Rate and Blood Pressure Spikes
Stress hormones raise your heart rate and tighten blood vessels. During depression or anxiety, these surges can happen many times a day. Even if they last only a few minutes, the repeated spikes add strain to your heart.
This is one way depression affects the body and contributes to physical illness. You might feel pounding, pressure, or short bursts of dizziness, which can be unsettling and mistaken for heart disease.
These changes do not always cause long-term heart problems, but they can worsen existing conditions. People with high blood pressure or heart risk need extra monitoring.
Weight Loss or Gain from Appetite and Metabolic Changes
Depression disrupts appetite signals, making you eat too little or too much. These swings affect your metabolism and energy levels. Sudden weight change is one reason depression can make you sick , because your body struggles to keep stable blood sugar and hormone balance. Eating too little lowers muscle strength, while eating too much raises inflammation and fatigue. Both patterns make daily tasks harder.
Doctors watch for these changes because appetite problems may signal a shift in the severity of depression. When mood improves, appetite usually stabilizes, but some people need help rebuilding a healthy pattern.
Hormonal Shifts That Mimic Physical Illness
Depression alters stress hormones, thyroid signaling, and reproductive hormones. These shifts cause symptoms that look like separate medical diseases. Fatigue, cold sensitivity, low libido, or menstrual changes may confuse you and your doctor. This is why depression affects the body in ways that reach far beyond mood.
Clinicians sometimes repeat hormone tests to confirm results over time. This prevents misdiagnosis and ensures you do not receive unnecessary medication. Treatment often focuses on restoring sleep, lowering stress, and improving mood, which naturally stabilizes hormones. When mood improves, many hormone-related symptoms fade.
Impact on Sexual Health: Libido, Energy, Performance
Low mood reduces desire, energy, and comfort during intimacy. Stress hormones interfere with arousal, and fatigue makes sexual activity feel draining. Medications may also affect sexual response for some people. These combined effects are another way depression affects the body and your relationships.
When sexual symptoms appear, doctors review mood, medications, and sleep patterns. Adjusting treatment often helps. Communication with your partner and clinician can reduce shame and confusion.
Blood Sugar Imbalances and Risks for Metabolic Conditions
Poor sleep and stress hormones interfere with how your body manages blood sugar. You may feel shaky, tired, or hungry even when you eat regularly. Over time this instability raises risk for metabolic issues. These shifts show how depression affects the body and can lead to long-term health concerns if untreated.
Monitoring patterns helps you and your doctor understand what triggers these swings. Stabilizing sleep, eating on schedule, and treating mood all reduce blood sugar fluctuations. For those with diabetes or prediabetes, combined care becomes even more important.
Emotional Stress Making You Physically Sick
Fight-or-Flight Overload and Cortisol Surges
When emotional stress stays high, your fight-or-flight system activates repeatedly. Cortisol surges raise heart rate, tighten muscles, and disrupt digestion. With time this overload explains how emotional stress making you physically sick becomes a daily reality. You may feel restless, sweaty, or shaky, even without a clear threat.
Clinicians see this pattern in anxiety and depression, especially when sleep is poor. Treatment aims to lower the body’s baseline stress level. Softer routines, grounding skills, and therapy help the nervous system switch off emergency mode.
Stress-Triggered Inflammation and Immune Suppression
Stress raises inflammatory chemicals and weakens some immune defenses. These shifts make infections more likely, and recovery often takes longer. This biological pattern is one reason depression can make you sick instead of just sad. You might notice more colds or slower healing during stressful episodes.
Because not everyone responds the same way, doctors evaluate lifestyle, sleep, and illness history before choosing treatment. Improving mood, movement, and sleep together often strengthens immunity.
How Prolonged Distress Increases Vulnerability to Infections
Long-term distress drains the body’s resources. Immune cells become less responsive, and inflammatory markers rise. This combination makes infections more frequent and symptoms more severe. You may catch viruses easily, or simple infections may feel harder to move past.
Early treatment for mood symptoms lowers this risk. Clinicians often monitor sleep patterns, appetite, and stress history to understand how mood and immunity interact. Recovery improves when both sides are treated.
Brain–Gut Axis: How Stress Activates Digestive Disorders
Your gut has a network of nerves that react quickly to stress. Signals from the brain change gut movement, sensitivity, and bacterial balance. These shifts create cramping, nausea, diarrhea, or IBS-like discomfort.
Treating gut symptoms alone often gives limited relief. When stress and mood improve, digestive symptoms usually settle. Doctors may combine diet guidance, sleep care, and therapy to help balance the gut-brain system.
Depression vs. Actual Illness
Overlapping Symptoms With Viral Or Chronic Conditions
Fatigue, sleep change, and body pain appear in both depression and many medical illnesses. You may find it hard to tell which cause sits behind your symptoms. When symptoms start slowly and match mood change, depression is likely; when they start suddenly, a medical cause is more likely.
Doctors compare timelines, exam findings, and basic labs to separate causes. Tests like blood counts, thyroid checks, and infection screens help decide whether mood or a virus is the main driver. This careful check prevents missed diagnoses and guides the right care.
When Physical Symptoms Signal A Separate Medical Issue
Some signs point away from mood and toward a medical illness. High fever, sudden focal weakness, severe and unexplained weight loss, or blood in stool or urine need urgent medical checks. If you have any of these, clinicians will investigate for infections, autoimmune disease, or cancer.
Telling your clinician about new, dramatic physical changes helps them choose the right tests quickly. You should not assume all new pain or fatigue is due to mood; timely testing can find treatable medical problems early.
Why Depression Makes Existing Illnesses Feel Worse
When you are depressed, you sleep poorly, move less, and may skip medications. These behaviors weaken recovery and amplify pain in chronic conditions like arthritis or diabetes. Low mood lowers your pain tolerance and reduces your drive to follow care plans.
Improving your mood often improves your ability to self-care. Treating depression boosts motivation, sleep, and activity, which helps control long-term illnesses and reduces their flare-ups. Addressing both mood and disease leads to better outcomes.
Red Flags Requiring Immediate Medical Evaluation
Certain signs need emergency care. Sudden chest pain, severe shortness of breath, fainting, sudden severe abdominal pain, or sudden limb weakness should lead you to urgent care or the emergency room. Do not delay because you suspect mood is involved.
If you or someone near you experiences these signs, seek immediate help. Emergency teams will rule out life-threatening causes first, then coordinate follow-up for mood and recovery once the urgent issue is addressed.
Treating Physical Symptoms of Depression
Evidence-Based Therapies That Improve Both Mood And Physical Health
Therapies like cognitive behavioral therapy change how you think about pain and stress. These approaches lower symptom focus, improve sleep, and increase activity, which reduces both mood and body complaints. Exercise programs with graded activity also cut pain and lift mood.
Mindfulness and paced physical rehabilitation show benefit in trials when added to standard care. Choosing therapy depends on access and symptoms, but evidence supports combining psychological treatment and activity to relieve both mood and bodily symptoms.
Medications That Reduce Pain And Regulate Mood
Some antidepressants alter pain pathways and ease aches while improving mood. Doctors usually select a medicine based on your symptoms, health history, and side effect risk. Dosage varies by age and condition, so clinicians adjust carefully over time.
Medication often helps most when combined with therapy and lifestyle changes. Follow-up visits let your doctor monitor effects and side effects and change the plan if pain or mood do not improve.
Lifestyle Changes Proven To Counter Physical Stress Damage
Regular, moderate movement reduces pain sensitivity and improves sleep. Consistent sleep times restore repair cycles and lower inflammation. A balanced diet with regular meals supports stable energy and immune function. Limiting alcohol and not smoking help your body heal faster.
When Combined Care (Mental + Physical) Is Essential
When symptoms cross systems, teams that include primary care, mental health, and physical therapy give the best results. These teams share records and align treatment goals so you do not get mixed messages. You benefit when mood, labs, and function are tracked together.
Ask your clinician for integrated care when pain, sleep, appetite, or heart symptoms co-occur with low mood. Joint plans reduce relapse and treat the root causes rather than only masking symptoms.
When to See a Doctor for Depression-Related Physical Symptoms
Persistent Pain That Interferes With Daily Life
If pain stops you from working, sleeping, or caring for yourself, seek a full medical review. Persistent pain often needs both medical testing and mental health treatment to break the cycle of pain and low mood.
Early, combined treatment reduces the chance that pain becomes chronic. A care plan may include drugs, therapy, exercise, and pacing strategies to restore function.
Severe Digestive Or Cardiovascular Symptoms
Ongoing vomiting, severe belly pain, black or bloody stools, chest pain, fainting, or severe shortness of breath need urgent evaluation. These signs may represent a separate medical emergency, not only mood changes.
Tell your doctor about every symptom clearly. Urgent testing prevents harm, and after acute issues are ruled out, clinicians can focus on mood-related contributors to ongoing discomfort.
Symptoms That Worsen Despite Treatment
If pain, fatigue, or gut symptoms increase while you follow treatment, ask for a re-evaluation. New tests, specialist referral, or a change in therapy may be needed. Worsening symptoms can mean a missed diagnosis or insufficient treatment.
Do not assume slow improvement is normal without review. A fresh assessment helps determine whether to intensify therapy, add a specialist, or investigate other causes.
What Doctors Evaluate During Assessment
Clinicians check vital signs, examine your heart and lungs, and order labs like blood counts, thyroid function, and inflammation markers as needed. They review medications, sleep, alcohol use, and stress history and assess mood with standard questionnaires.
This broad approach finds hidden medical issues and measures how mood links to body signs. It also sets a clear plan so you and your clinician track progress and adjust care over time.
FAQ
Why Does Depression Cause Physical Symptoms?
Mood shifts alter hormones, sleep, and nerve signals that control pain, appetite, and energy, so emotional problems show up as real physical symptoms. Treating mood often eases these body changes.
Can Depression Weaken The Immune System?
Long stress and major depression change immune signaling, raising inflammation and reducing some immune responses, which makes infections more likely and slows healing in many people. Evidence is strong but varies by person.
How Long Do Physical Symptoms Of Depression Last?
Duration depends on treatment and severity. With care, many people improve in weeks to months. Untreated cases often persist and can take longer to recover. Early treatment shortens recovery.
Can Depression Make Chronic Conditions More Painful?
Yes. Depression lowers pain tolerance and reduces self-care, which worsens chronic illnesses and raises flare-ups. Treating mood helps reduce pain and improve disease management.
What Physical Symptoms Signal Severe Depression?
Severe sleep loss, large weight change, constant disabling pain, loss of daily function, or suicidal thoughts are red flags that need immediate professional help. Do not ignore these signs.
Can Depression Cause Dizziness Or Lightheadedness?
Yes. Poor sleep, blood sugar swings, low blood pressure, and medication effects can cause dizziness. If sudden or severe, seek medical evaluation to rule out other causes.
How Do I Know If My Symptoms Are From Stress Or A Medical Issue?
Doctors use history, exams, and tests to separate mood-related symptoms from medical disease. Give clear timelines and symptom details so clinicians can decide which tests are needed.
Can Treating Depression Reduce Body Pain?
Yes. When mood improves, pain pathways calm and function returns. Therapy, medication, and lifestyle changes together yield the best pain reduction for mood-related pain.
Does Anxiety Combined With Depression Worsen Physical Illness?
Yes. Coexisting anxiety raises arousal, cortisol, and muscle tension more than depression alone, increasing pain, gut trouble, and immune disruption. Treating both conditions reduces overall physical harm.
What Is The Fastest Way To Relieve Physical Symptoms Of Depression?
Short-term relief comes from steady sleep, slow breathing exercises, short walks, hydration, and contacting a clinician for a tailored plan. These steps lower stress hormones and ease symptoms quickly.












Leave a Comment