Hemorrhoids are swollen veins in the lower rectum and anus that can bleed, itch, or feel sore when you pass stool. Doctors treat them with simple steps like fiber, warm sitz baths, stool softeners, and, in tougher cases, surgical procedures such as banding or sclerotherapy.
To know if hemorrhoids can fade without treatment depends on the type and severity. Mild cases often settle when stool becomes softer, and you stop straining, so yes, hemorrhoids can heal on their own in many early stages.
External hemorrhoids may shrink on their own if there is no blood clot, though thrombosed ones take longer and can be painful. Internal hemorrhoids can improve with better bowel habits, but larger ones that slide out usually need medical support.
Can Hemorrhoids Heal On Their Own?
When Mild Hemorrhoids Typically Resolve
Small internal hemorrhoids that only bleed a little or itch can improve in a few days to a couple of weeks when stool is soft, and you do not strain. There is no exact timeline, but you may feel better once constipation is treated and toilet time is shorter. For these mild cases, hemorrhoids can heal on their own , as long as you support your bowels properly.
Why Hemorrhoids Sometimes Come Back
Even when symptoms fade, the stretched vein that formed your hemorrhoids usually stays weak. If you go back to low fiber meals, long sitting, or heavy lifting, pressure rises again in the anal veins and a new flare starts. Long-term constipation and long toilet sitting with repeated piles can lead to new hemorrhoids .
How Long does Healing Normally take?
Many mild flares of hemorrhoids settle within about a week, while larger external lumps can take several weeks to shrink and feel comfortable. If pain, a lump, or bleeding lasts longer than one month or suddenly gets worse, you should see a doctor so they can rule out other causes like anal fissures (small tears) or bowel disease.
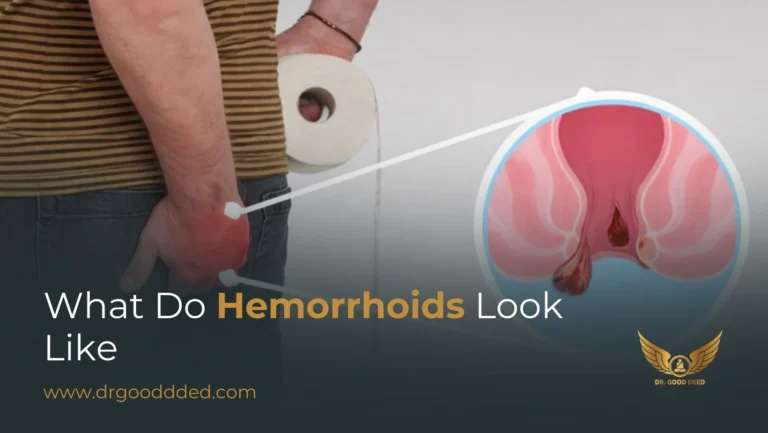
Do External Hemorrhoids Go Away?
External hemorrhoids form under the skin at the anal opening and feel like a soft or firm bump. These bumps can make it hard to sit or clean after a bowel movement. Small, non-thrombosed external piles often fade over one to two weeks with careful home care, while those with a blood clot take longer but can still improve without surgery in many cases.
Thrombosed vs Non Thrombosed External Hemorrhoids
A thrombosed (blood clot-filled) external hemorrhoid has a clot trapped in the vein. It shows up suddenly, hurts a lot, and may look blue or purple. A non-thrombosed one grows more slowly and causes aching or itching instead of sharp pain. Both kinds are hemorrhoids . The clot mainly changes how strong the pain feels and how long the lump takes to shrink.
What Speeds Up Healing For External Hemorrhoids
Good self-care treatment for haemorrhoid problems focuses on lower pressure and calmer skin. Warm sitz baths, where you sit in a few inches of warm water for 10 to 15 minutes, can ease swelling and soreness by relaxing the area and improving blood flow.
Short ice packs wrapped in a cloth, gentle cleaning with water rather than harsh dry wiping, and avoiding long toilet sessions can also support the healing of external hemorrhoids and make daily life less uncomfortable.
When External Hemorrhoids May Require Treatment
You should see a doctor if an external lump gets much bigger, if pain is severe, or bleeding is heavy or keeps coming back. Medicines and office procedures are best used when hemorrhoids do not settle with home care or flare again and again, or when symptoms stop you from sitting, working, or sleeping properly.
Do Internal Hemorrhoids Go Away?
Internal hemorrhoids sit inside the rectum and often cause painless, bright red blood on the stool or paper. Small internal piles may shrink when you soften your stool and reduce pressure, but larger ones that slip out of the anus tend to stay unless treated.
How Internal Hemorrhoids Behave Differently
Internal hemorrhoids have fewer pain nerves than the skin outside, so they can bleed a lot without much soreness. Early-stage internal piles often respond to fiber, enough water, and less straining, while later stages that prolapse (slide out of place) often need procedures such as rubber band ligation (a tight band to cut blood flow) or injection therapy called sclerotherapy (a medicine that scars the vein).
Symptoms That Indicate Persistence
Signs that internal hemorrhoids are not going away include frequent bleeding, a feeling of fullness or pressure, mucus on the stool, or tissue that bulges out every time you pass stool.
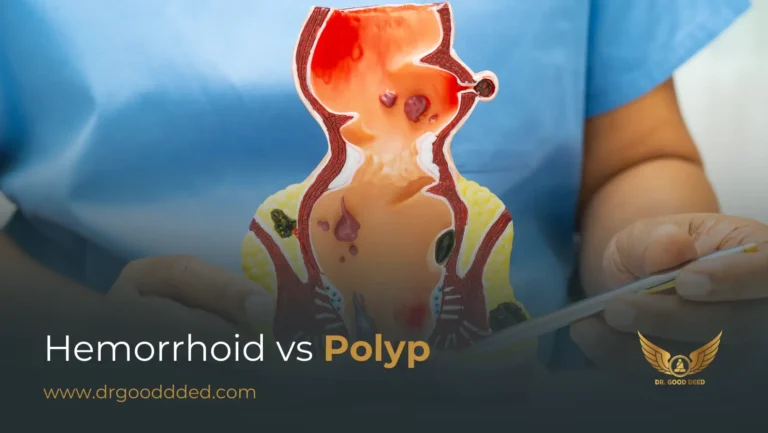
If these problems last for several weeks and you still wonder whether internal hemorrhoids go away in your case, doctors usually advise an exam or a short scope test to rule out other rectal diseases such as polyps or tumors.
Treatment Options For Recurring Internal Hemorrhoids
When internal hemorrhoids bleed often or prolapse again and again, doctors may suggest office treatments such as rubber banding, sclerotherapy, or infrared coagulation (heat used to seal the vein). These methods cut off blood flow to the swollen veins so they slowly shrink over time. You may feel good relief, but results vary from person to person, so following up with your own doctor is important.
Hemorrhoid Self-Care Treatment
Good daily care can calm many hemorrhoids and sometimes stop a flare from getting worse. Doctors from Mayo Clinic and Harvard list simple steps as first-line help, before any procedure.
Evidence Based Home Remedies That Work
Warm sitz baths help a lot. You sit in warm water up to your hips for 10 to 15 minutes. This relaxes the anal muscle and improves blood flow, so swollen hemorrhoids feel less tight and sore.
Soft stool is just as important. A high fiber diet with fruits, vegetables, beans, and whole grains makes stool bulky yet soft, so it passes without strain. Adults need about 25 to 35 grams of fiber each day, but your exact need can differ.
You can talk with your doctor about fiber supplements and stool softeners. Doctors usually adjust them based on your age, health, and other medicines. This kind of self-care treatment for haemorrhoid pain reduces pressure instead of only covering symptoms.
Lifestyle Habits That Prevent Flare-Ups
Daily habits often decide if hemorrhoids stay quiet or keep flaring. Long sitting on the toilet, especially with a phone, increases rectal pressure. New studies link this habit with a higher risk of hemorrhoids because you sit longer than needed.
Try to go when you feel the urge, finish, then leave the toilet. Do not sit and scroll. Move your body during the day. Short walks help your bowel move and lower pressure in the pelvic veins. Drink water often so your stool does not turn dry and hard. This steady self-care treatment for hemorrhoid trouble often works better than quick fixes.
Daily Routine To Reduce Swelling And Discomfort
You can follow a simple plan. Start your day with water and a fibre-rich breakfast. When you use the toilet, keep your feet flat or on a small footstool to open the rectum (the last part of the bowel). Do not push hard or hold your breath.
Clean the area gently with water or soft wipes. Avoid harsh soap. In the evening, take a warm sitz bath if your hemorrhoids feel sore. Use creams or pain tablets only as your doctor advises. This routine supports healing, whether haemorrhoids can heal on their own or you also need medical care.
Duration Of Hemorrhoid Flare Ups
Typical Timeline For Flare-Ups To Settle
There is no exact clock for hemorrhoids , but experts agree on rough ranges. Small internal or external flares often calm within a few days when stool is soft and strain is low. Thrombosed external lumps, which contain a clot, may hurt for two or three weeks while the body slowly absorbs the clot.
Signs Your Flare Up Is Taking Longer Than Normal
You should see a doctor if strong pain, swelling, or bright red bleeding from hemorrhoids lasts beyond one month. An earlier review is wise if symptoms disturb your sleep, work, or daily tasks. Very long flares can also hide other anal problems that look similar on the outside.
When Inflammation Becomes Chronic
If one flare fades and another starts soon, inflammation can become long-lasting. The tissues stay thick and tender much of the time. At this stage, home care still helps, but it may not be enough to shrink hemorrhoids . Doctors then review your case and talk about other options.
Chronic Hemorrhoids Causes
Why Hemorrhoids Fail To Resolve Naturally
Researchers link most chronic hemorrhoids causes to repeated high pressure in the rectal veins. Constipation, hard stool, long sitting, and low fiber diets all increase that pressure.
Pregnancy, heavy lifting, and extra body weight also add strain. When these pressures stay for years, the supporting tissue around the veins stretches and loses strength, so hemorrhoids remain even when one flare ends.
Risk Factors That Worsen Chronic Hemorrhoids
You face more risk if you often ignore the urge to pass stool, use the toilet as a reading spot, or eat mostly processed food. Sedentary life, low fiber intake, and long sitting are linked with more hemorrhoids and worse grades. These chronic hemorrhoids often build slowly, so you may not notice them until symptoms become severe.
When To Consider Medical Evaluation
You should get a medical check if bleeding or pain keeps coming back despite careful home steps, or if you have a family history of bowel cancer. Doctors will look for hemorrhoids and also check for polyps (small growths) or other diseases. They may also advise procedures if lifestyle changes alone fail.
When Hemorrhoids Do Not Go Away On Their Own
Warning Signs Of Complications
You need urgent care if you notice sudden, strong pain with a very hard lump, heavy bleeding, fever, or pus from the anal area. These signs can point to a big clot, strangulated tissue, or infection around hemorrhoids .
When Hemorrhoids Need Medical Procedures
If your hemorrhoids still bleed, slip out, or hurt after many weeks of proper self-care, doctors may suggest office treatments or surgery. They choose methods based on the grade, size, and whether the piles are internal, external, or both.
Long-Term Management Strategies
Even after treatment, you still need healthy bowel habits. Fiber, water, movement, and limited toilet time remain important. Regular follow-up lets your doctor catch new problems early and adjust your plan if hemorrhoids start to come back.
Treatment Options If Hemorrhoids Don’t Go Away
Office Based Treatments (Banding, Sclerotherapy, Infrared)
Office treatments aim to cut blood flow to internal hemorrhoids so they shrink. Rubber band ligation places a tiny elastic band at the base. Sclerotherapy uses a medicine injection to scar the vein. Infrared coagulation uses a short heat pulse to seal the tissue.
Studies suggest banding often gives the strongest long-term control for grades two and three, but it can hurt more for a short time and may cause minor bleeding. Evidence directly comparing all techniques is limited, so doctors often choose based on experience and your exact findings.
Surgical Treatments For Severe Or Chronic Hemorrhoids
If office options fail or hemorrhoids are large, mixed internal and external piles, surgery may help. Standard hemorrhoidectomy removes extra tissue. Stapled hemorrhoidopexy uses a ring-shaped stapler to lift internal piles and cut blood supply. A surgeon picks a method after a full exam and discussion of risks, pain, and recovery time.
Expected Recovery After Each Treatment
After banding or other office care, many people feel pressure or mild pain for a few days. Light bleeding around day seven is common when the banded tissue falls off. After full surgery, recovery often takes one to two weeks or more, with pain slowly improving. Doctors adjust pain control and stool softening for each person, since there is no single plan for everyone.
When To See A Doctor For Hemorrhoids
Red Flag Symptoms That Require Urgent Attention
Go to urgent care or an emergency room if you have heavy bleeding, weakness, fainting, severe anal pain, or trouble passing stool or gas. These problems can come from hemorrhoids , but also from other serious diseases that need fast care.
When Bleeding Is Not Normal
Small streaks of bright red blood on paper can fit with hemorrhoids . Dark red clots, blood mixed with stool, or black tar-like stool can mean bleeding higher in the bowel. These signs always need medical review, not only home care.
How Doctors Diagnose Hemorrhoids Vs Other Conditions
Your doctor will ask about your bowel habits and then examine the anus. They may do a gentle finger exam, then use a short scope called an anoscope to view internal hemorrhoids . If bleeding is unclear or if you have risk factors, they may also advise a colonoscopy to look at the whole large bowel.
Prevention Strategies To Avoid Recurrence
Diet And Fiber Intake Recommendations
A fibre-rich eating plan helps prevent new hemorrhoids and also supports healing. Try to include plant foods with each meal and drink water throughout the day, not just at night. Doctors sometimes give a fiber chart so you can track how much you get.
Bowel Habits That Prevent Strain
Respond to urges early; do not wait. Keep toilet visits short. Avoid reading or using your phone there, because longer sitting raises anal vein pressure and may lead to more hemorrhoids over time.
Workplace And Lifestyle Adjustments
If you sit a lot for work, stand up and walk for a minute every hour. If you lift heavy items often, ask your doctor or a trainer how to use a safer technique. These small shifts lower many chronic hemorrhoids causes that build silently over the years.
FAQ
How Long Do Hemorrhoids Usually Take To Go Away?
Mild hemorrhoids often improve within a week when stool is soft and you avoid strain. Larger external lumps or clots can take several weeks to flatten, so steady home care and follow-up matter.
Can Hemorrhoids Heal Without Treatment?
Some small hemorrhoids improve with time, fiber, and better toilet habits. Still, you should not rely only on hemorrhoids healing on their own, if bleeding is strong or frequent or if you have risk factors.
How Do I Know If My Hemorrhoids Are Getting Worse?
You should worry if hemorrhoids bleed more often, hurt more, or start to bulge out and stay out. Trouble cleaning, mucus, or leaking stool also signals that the disease is progressing.
Will External Hemorrhoids Shrink On Their Own?
Small external hemorrhoids can shrink with good home care and less toilet strain. If pain is severe, an exam helps guide the next steps.
Do Internal Hemorrhoids Disappear Without Procedures?
Early internal hemorrhoids sometimes settle with fiber and lifestyle change. When prolapse or repeated bleeding continues, internal hemorrhoids doesn’t go away without banding or other treatment.
What Makes Hemorrhoids Last Longer Than Normal?
Hard stool, low fiber intake, and long toilet sitting all keep hemorrhoids irritated. Extra body weight, pregnancy, and some chronic causes of hemorrhoids, like sedentary life, can also stretch veins and slow healing.
Can Chronic Hemorrhoids Be Permanent?
Long-standing hemorrhoids may not shrink on their own, but they are rarely hopeless. With a mix of home care, office treatments, and sometimes surgery, most people gain long-term control of symptoms.
What Is The Fastest Way To Reduce Hemorrhoid Swelling?
You usually get the quickest relief by combining a short ice pack, a warm sitz bath, and stool softening. These steps lower pressure on hemorrhoids while your doctor decides if more treatment is needed.
When Does Bleeding From Hemorrhoids Become Concerning?
Bleeding from hemorrhoids becomes concerning when it is heavy, repeated often, or comes with weakness, faint feeling, or black stool. At that point, you need a prompt medical review.
Can Lifestyle Changes Alone Prevent Future Hemorrhoids?
For many people, fiber, water, movement, and healthier toilet habits greatly cut new hemorrhoids and flares. Some people still need procedures, but lifestyle change almost always improves comfort and bowel health.








Leave a Comment