Stress is usually not the direct cause of blood in stool . But stress pushes existing problems harder. It can trigger constipation or diarrhea, raise gut sensitivity, and flare illnesses that already tend to bleed.
When those flare, you may see blood in stool on the paper, in the bowl, or mixed with stool. That is why any new blood in stool needs medical review, even if you feel sure stress is to blame.
Stress hormones change how your brain and gut talk to each other. They can slow the bowel in some people and speed it up in others. Both patterns can aggravate hemorrhoids, anal fissures, inflammatory bowel disease, or ulcers. These conditions are the real source of most blood in stool , not stress alone. Colon cancer and active inflammatory bowel disease can first show up as blood in stool , sometimes with few other symptoms. So you should never ignore this sign.
Can Anxiety Cause Blood in Stool?
Anxiety itself does not cause blood in stool . Still, it can change how often you go, how hard you strain, and how strongly you feel gut pain. These shifts can set the stage for blood in stool when you already have hemorrhoids, a tiny tear, or active bowel disease.
How Anxiety Triggers Gut Inflammation And Irritation
When you feel anxious, your body releases stress hormones like adrenaline and cortisol. These chemicals alter blood flow and bowel movement. People with irritable bowel syndrome (IBS) often have worse cramps and looser stools when stress is high. Stress makes IBS symptoms flare, but it does not cause IBS by itself.
IBS usually does not cause blood in stool , and bleeding is one of the signs that makes doctors think about inflammatory bowel disease (IBD) instead of IBS. However, frequent trips to the toilet and repeated wiping during IBS flares can irritate the skin around the anus. If the skin cracks or small veins swell, you may notice light streaks of blood in stool .
Stress Hormones And Their Effect On Bowel Function
Stress hormones can speed up or slow down your bowel. If your bowel speeds up, you may have many loose stools in a day. The skin around the anus gets sore from wiping, so even a small tear can bleed.
If your bowel slows down, stool becomes harder and drier, and you strain more. Hard stools and straining are key triggers for hemorrhoids and anal fissures, and both are common reasons for blood in stool in adults.
When Anxiety-Related Bleeding Is Unlikely
Bleeding is unlikely to be mainly anxiety-related when it is heavy, when it turns stool black and sticky, or when it comes with weight loss, fever, or strong abdominal pain. These alarm signs point to structural diseases such as inflammatory bowel disease, serious infection, ulcers, or cancer. In that setting, blood in stool needs urgent medical review, not just self-care for anxiety symptoms.
Causes of Stress-Induced Blood in Stool
Stress behaves more like a switch that worsens problems that already exist. It also nudges you toward habits that are rough on the gut, such as poor sleep, less movement, and fast, low-fiber meals. Over time, these changes make constipation, hemorrhoids , and small tears more likely, and those are some of the most frequent causes of blood in stool in otherwise healthy people.
Stress-Induced IBS Flares And Mucosal Irritation
In irritable bowel syndrome, the bowel looks normal on tests, but its nerves and muscles are extra sensitive. Stress can make IBS symptoms more frequent and more intense. During a flare, you may have extra gas, cramping, and urgent trips to the toilet.
Constant wiping and straining can irritate the inner lining near the rectum, called the mucosa (the moist inner surface). While IBS itself does not usually cause blood in stool , the irritation it creates around the anus in a stress flare can lead to minor bleeding from small cracks or swollen veins.
How Chronic Stress Worsens Inflammatory Bowel Conditions
Inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis, involves real inflammation and ulcers in the gut lining. Many people with these conditions notice that flares often follow long periods of stress or poor sleep, although studies show that stress is a trigger, not the root cause.
Ongoing stress can affect immune signals in the gut and make inflammation harder to control. During a flare, you may notice rectal bleeding, diarrhea, and cramping. Doctors focus on treating the inflammation with medicine first, then help you work on stress control so flares and blood in stool become less frequent.
Indirect Causes: Dehydration, Poor Diet, And Constipation
Stress often changes your daily habits in quiet ways. You may drink more coffee and less water, skip meals, or choose low-fiber snacks. You might sit for long hours and ignore the urge to go to the toilet. These patterns lead to hard, dry stools and constipation.
Hard stools scrape the anal lining and make you strain, which raises the risk of hemorrhoids and tiny tears called fissures. Both are very common and treatable sources of bright red blood in stool on the toilet paper.
Stress And Hemorrhoid Flare-Ups
Stress alone does not create hemorrhoids, but it strongly fuels stress and hemorrhoid flare-ups . When you feel tense, your bowel habits often change. You may rush toilet time, hold stool for later, or sit for long periods. These patterns increase pressure in the rectal veins.
Over time, this pressure makes the veins swell into hemorrhoids, which become one of the most common sources of bright red blood in stool .
How Stress Contributes To Constipation And Straining
Ongoing stress can slow the bowel in some people. You might drink less water, eat less fiber, and move less during the day. Stool sits longer in the colon, gets drier, and becomes hard to pass. To get it out, you push harder and strain.
Chronic constipation and straining are key risk factors for hemorrhoids and fissures, both of which can cause blood in stool . This chain of events explains why much of blood in stool comes down to stress-driven constipation and straining.
Why Hemorrhoids Bleed During Flare-Ups
Hemorrhoids are covered by thin, delicate tissue. During stress and hemorrhoid flare-ups , this tissue becomes even more fragile due to swelling and repeated rubbing with hard stool or dry toilet paper.
A single bowel movement can scrape the surface and open tiny vessels, so you see bright red blood in stool on the paper or coating the stool. The bleeding is often painless, which can fool you into thinking it is not serious. Clinics note that any new rectal bleeding should still be checked, even if hemorrhoids seem likely.
Signs Your Bleeding Is Hemorrhoid-Related
Bleeding from hemorrhoids usually appears as bright red drops or streaks that seem to sit on the surface of the stool rather than mixed through it. You may feel itching, swelling, or a soft lump at the anus.
Pain is often mild, unless a clot forms inside the hemorrhoid. Even when these signs fit, doctors advise at least one exam to confirm that hemorrhoids are the true source of blood in stool , since more serious disease can look similar at first.
Stress-Induced Digestive Bleeding
Stress interacts with other risks, such as infection with H. pylori bacteria or long-term use of pain drugs from the NSAID group, and causes digestive bleeding. Most stomach and upper gut ulcers come from H. pylori or NSAIDs, with stress acting as a weaker but real factor that can raise bleeding risk in people who already have these problems.
When Stress Leads To Gastric Or Intestinal Irritation
During strong stress, your body produces more stomach acid and changes how fast your stomach empties. This can irritate the stomach lining, causing gastritis, which means inflammation of the stomach wall.
People with gastritis may feel burning pain high in the abdomen, nausea, or fullness. If the irritated lining starts to ooze blood, stools can turn dark and tar like.
Ulcer Flare-Ups Triggered By Stress
If you already have a peptic ulcer (a sore in the stomach or upper small intestine), stress can make symptoms stronger and increase the chance of bleeding. Stress can raise ulcer risk in both H. pylori-related and non H. pylori ulcers, but it still acts more like a trigger than a root cause.
When an ulcer bleeds, you may vomit blood or pass black, sticky stool rather than bright red blood in stool . Doctors usually confirm ulcers with endoscopy, then treat the infection or drug cause, and may also guide you on stress control so that future ulcer bleeding is less likely.
When Stress Worsens Existing GI Conditions
Long-term gut conditions, such as reflux disease, inflammatory bowel disease, and functional bowel disorders, show a clear stress link. Symptoms like pain, diarrhea, and urgency tend to rise during hard life periods.
In inflammatory bowel disease, stress does not cause the disease, but it can worsen flares, which may lead to visible blood in stool . That is why good care combines medical treatment of the gut with help for sleep, mood, and coping skills.
Does Stress Cause Rectal Bleeding?
Rectal bleeding almost always comes from a physical problem in the lower gut or anus. Stress shapes how that problem behaves, how often it flares, and how you feel it, but it rarely acts alone.
Situations Where Stress Can Indirectly Cause Rectal Bleeding
Stress can lead to poor toilet habits, which then cause bleeding. You might strain during constipation or have frequent bouts of diarrhea. Both situations irritate the anal canal. Over time, hemorrhoids or fissures can form. When these bleed, you see blood in the stool .
Conditions Commonly Mistaken For Stress-Related Bleeding
You may think your bleeding must be from stress or hemorrhoids, yet tests later show colon polyps, inflammatory bowel disease, or even cancer. Cancer groups warn that blood in stool and lasting changes in bowel habits are classic early signs of bowel cancer, especially if you are over 45 or have a family history.
Red Flags Requiring Immediate Evaluation
You should seek urgent medical care if you pass a large amount of blood, feel dizzy or faint, or see black, tar-like stools. Red flags also include weight loss without trying, ongoing fatigue from possible anemia, and a clear change in bowel habit that lasts more than a few weeks.
In these situations, the concern goes far beyond stress-induced rectal bleeding and moves toward finding a serious cause quickly.
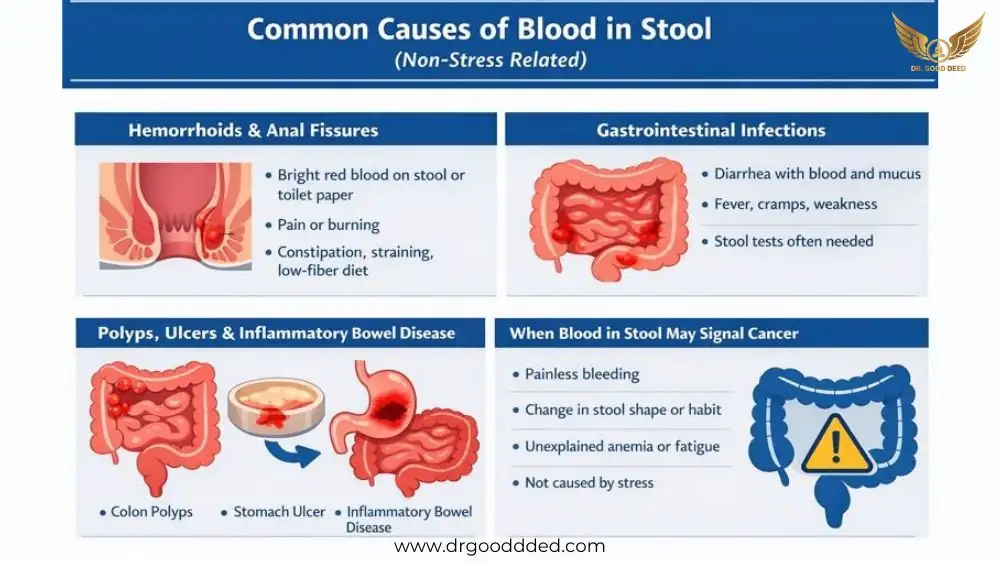
Other Common Causes Of Blood In Stool (Non-Stress Related)
Hemorrhoids And Anal Fissures
Hemorrhoids and anal fissures are the two leading minor causes of blood in stool . Hemorrhoids are swollen veins in the rectum or anus. Anal fissures are small tears in the anus, often caused by passing hard stool. Both can cause bright red blood in stool , especially on the paper, and often link to constipation, straining, and low fiber diets.
Gastrointestinal Infections
Bacterial or viral gut infections can damage the bowel lining and lead to diarrhea mixed with mucus and blood in stool . You may also have fever, cramps, or feel very unwell. Doctors often use stool tests to check for infection, especially if symptoms last more than a few days or if you have traveled recently.
Polyps, Ulcers, And Inflammatory Bowel Disease
Colon polyps are small growths that may bleed and can sometimes change into cancer over time. Ulcers in the stomach or small intestine can bleed and cause black stool.
Inflammatory bowel disease, like Crohn’s disease and ulcerative colitis, causes long-term inflammation and repeated blood in stool during flares. None of these are caused by stress alone, but stress can make the symptoms worse and the bleeding more frequent.
When Blood In Stool May Signal Cancer
Cancer groups warn that colon and rectal cancer often show up first as painless blood in stool , a slow drop in blood count, or a change in stool shape or habit. These signs can be easy to overlook, especially in younger adults who assume stress or hemorrhoids are the cause.
How To Diagnose The Cause Of Blood In Stool
Medical History And Physical Exam
When you see a doctor for blood in stool , the first steps are careful questions and a physical exam. The doctor asks when you saw blood, how it looked, how often it appears, and if you have other symptoms like pain, diarrhea, constipation, weight loss, or fatigue.
They also ask about medicines and family history of gut disease or cancer. A gentle rectal exam can find hemorrhoids, fissures, or other problems near the anus.
Stool Tests, Blood Tests, Imaging
Stool tests can look for hidden blood in stool , infection, or signs of inflammation. Blood tests check for anemia and infection markers. In some cases, imaging such as CT scans or ultrasound helps find issues in the deeper bowel or nearby organs. Guidelines stress that tests should match your symptoms and risk factors, rather than follow a one-size-fits-all all plan.
When Colonoscopy Is Recommended
For many adults with unexplained blood in stool , colonoscopy is the main test doctors use. A thin tube with a camera is passed through the rectum to view the colon lining directly.
The doctor can remove small polyps, take samples from suspicious areas, and sometimes treat bleeding spots. Expert groups recommend prompt colonoscopy for people over 50 with new rectal bleeding, or earlier if there are strong risk factors.
When To See A Doctor About Blood In Stool
Persistent Or Severe Bleeding
You should see a doctor if blood in stool continues for more than a few days, returns again and again, or seems to be more than a small streak. Even if you think stress or hemorrhoids are to blame, lasting bleeding needs a clear diagnosis so that serious causes are not missed.
Associated Symptoms: Pain, Fever, Diarrhea
If blood in stool comes with belly pain, fever, frequent diarrhea, or feeling very unwell, you may have an infection or an active inflammatory condition. These situations often need stool tests, blood work, and sometimes hospital care for fluids or stronger medicine.
When Emergency Care Is Needed
Emergency care is needed if you pass large clots, feel dizzy or faint, see black tar-like stool, or notice rapid heartbeat with blood in stool . These are signs of heavy bleeding in the gut, which can be life-threatening if not treated quickly.
FAQ
Can Stress Cause Blood In Stool?
Stress does not directly cut the bowel, but it changes bowel habits and worsens hemorrhoids, fissures, ulcers, and inflammatory bowel disease. These conditions are the real sources of blood in stool .
Can Anxiety Trigger Digestive Bleeding Or Irritation?
Yes, anxiety can change gut movement, increase cramps, and cause diarrhea or constipation. These changes irritate the anal area and can make small injuries bleed, which leads to visible blood in stool .
How Does Anxiety Affect Gut Inflammation And Bowel Function?
Anxiety activates stress hormones that alter gut movement and immune signals. In people with IBS or IBD, this can worsen pain, urgency, and sometimes bleeding, turning silent disease into blood in stool episodes.
How Do Stress Hormones Influence Bowel Habits?
Stress hormones may slow your colon, causing constipation and straining, or speed it up, causing loose stools. Both patterns increase irritation, so blood in stool, which is often stress-related, reflects these habit shifts.
When Is Bleeding Unlikely To Be Related To Stress?
Bleeding is less likely to be connected to stress when it is heavy, turns stools black, or comes with weight loss, anemia, or severe pain. These warning signs require urgent checks for cancer or major disease beyond stress-induced digestive bleeding .
What Are Stress-Related Causes Of Blood In Stool?
Stress-related paths include constipation with straining, diarrhea with frequent wiping, flares of hemorrhoids, fissures, IBD, and ulcer flares. All can turn minor gut issues into visible blood in stool .
How Does Stress Worsen IBS Flares Or Mucosal Irritation?
Stress makes the gut more sensitive and changes muscle movement. IBS flares bring cramps, gas, and frequent stool, which irritate the rectal lining. That irritation sometimes causes small tears and blood in stool .
Can Chronic Stress Aggravate Inflammatory Bowel Conditions?
Yes, long-lasting stress can upset immune balance in the gut and increase flares of Crohn’s disease and ulcerative colitis. During flares, ulcers form and may bleed, leading to blood in stool .
Can Dehydration, Poor Diet, Or Constipation From Stress Cause Bleeding?
Yes, low water intake and low-fiber food from stressful living cause hard stools and constipation. Straining and scraping from these stools can create hemorrhoids or fissures that bleed and cause blood in stool .
How Does Stress Contribute To Constipation And Straining?
Stress can make you delay toilet visits, tighten pelvic muscles, and choose fast, low-fiber meals. These habits slow bowel movements and harden stool, so you strain more and risk stress and hemorrhoid flare-ups and bleeding.
Why Do Hemorrhoids Bleed More During Stress Flare-Ups?
During stressful times, constipation, long sitting, and poor diet often combine. Swollen hemorrhoids then face more pressure and friction when you pass stool, so they tear more easily and cause bright red blood in stool .
Can Anxiety Cause Blood In Stool?
No. Anxiety changes your bowel habits and does not cause direct damage to your bowel movements. Anxiety triggers constipation, diarrhea, and straining, which then lead to hemorrhoids, fissures, and bleeding.
Is Stress-Induced Digestive Bleeding Always Serious?
Some stress-induced digestive bleeding comes from small hemorrhoids or fissures and may stop with better habits. But because ulcers, IBD, and cancer can look similar, doctors still recommend proper checks for any ongoing blood in stool .
Does Stress Cause Rectal Bleeding Directly Or Indirectly?
Stress indirectly causes rectal bleeding . Stress alters bowel speed, diet, and habits, which then lead to physical injuries like hemorrhoids, fissures, or ulcer flares that bleed.









Leave a Comment