Stress affects your menstrual cycle by changing how your brain, hormones, and ovaries talk to each other. When stress hormones stay high, they can delay ovulation, lengthen or shorten your cycle, and change how heavy or painful your period feels. Doctors see stress as one of several common reasons for irregular or missed periods, along with pregnancy, thyroid problems, PCOS, and weight changes.
Researchers have linked high stress with anovulation (no egg release), longer or shorter cycles, worse PMS, and more painful periods, although not every study finds the same result. This means stress affects your menstrual cycle in many people, but not in the exact same way for everyone.
How Stress Affects Your Period
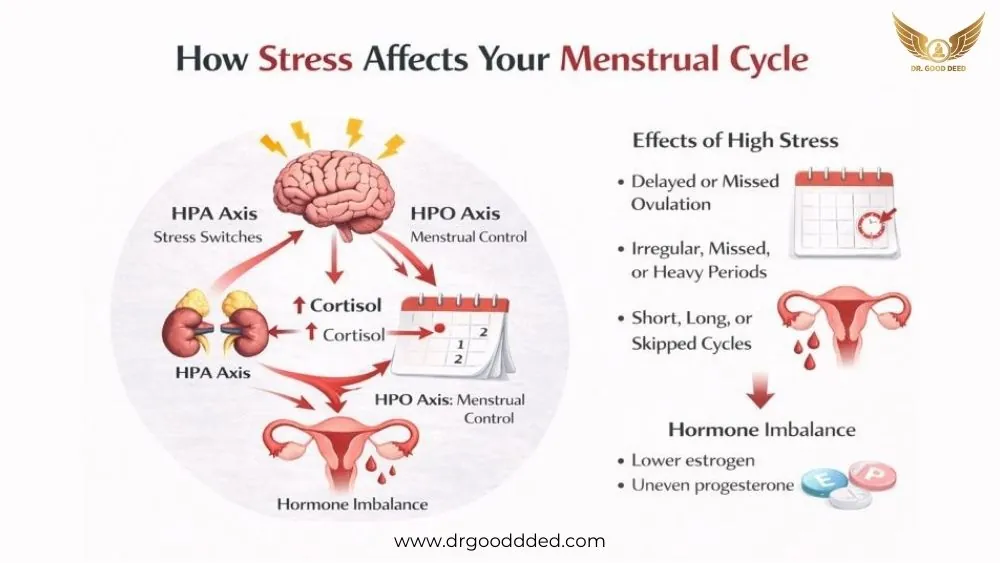
Your menstrual cycle depends on a control loop between your brain, pituitary gland, and ovaries. This is called the HPO axis (hypothalamic-pituitary-ovarian axis). When you are under pressure, your body turns on the HPA axis (hypothalamic pituitary adrenal axis). That makes cortisol, the main stress hormone. High cortisol can disturb the HPO axis, so stress affects your menstrual cycle through both the brain and the adrenal glands.
How Cortisol Interferes With Reproductive Hormones
Under calm conditions, your hypothalamus releases GnRH (gonadotropin-releasing hormone). GnRH tells your pituitary to release LH and FSH. These hormones tell your ovaries when to grow follicles, release an egg, and make estrogen and progesterone.
When stress is high, your adrenal glands release extra cortisol. Long-term stress can disturb this hormone chain and may reduce or change LH and FSH signals.
Over time, this may cause lower estrogen at some points, uneven progesterone after ovulation, or both. Many doctors describe this as stress and hormone imbalance , since the problem is not only in the uterus but in the full hormone control system.
Effects On Ovulation, Cycle Length, And Flow
A normal cycle for most people is roughly 21 to 35 days. The average is close to 28 or 29 days, but there is a wide normal range. Ovulation usually happens in the middle.
When stress affects your menstrual cycle , ovulation may happen later than usual or may not happen that month. If ovulation is late, your period often comes late. If you do not ovulate, you may skip a bleed or have only light spotting. High perceived stress is linked with longer or more irregular cycles, while others show weaker links.
You might notice that stress affects period flow as well as timing. For some people, the lining builds up longer and then sheds with heavier bleeding and more clots. For others, hormone signals are weak, so the lining stays thin, and bleeding is very light.
Differences Between Short-Term And Chronic Stress
Short-term stress can come from exams, a big work deadline, a family event, or travel. In many people, this kind of stress may only shift ovulation by a few days. Then stress affects your menstrual cycle for one cycle, and things settle when life calms down.
Chronic stress lasts for weeks or months. It can come from money problems, care duties, unsafe housing, long work hours, or ongoing illness. Chronic psychological stress can disturb ovarian function and is linked with more frequent anovulation and irregular cycles, although not all people respond the same way.
Can Stress Delay Your Period?
Yes. Doctors at major centers such as Mayo Clinic and Cleveland Clinic state that stress can change hypothalamus’ function and delay ovulation or stop it for a time. When ovulation shifts, stress affects your menstrual cycle, and your bleed often comes later. Some people even miss one or more periods during very stressful times.
Why Periods May Come Late During High Stress
Your body sees strong stress as a signal that the environment might not be safe for pregnancy. It moves energy toward basic survival and away from reproduction. High cortisol can blunt the normal LH surge that triggers egg release.
If there is no LH surge, there is no ovulation. If there is no ovulation, stress affects your menstrual cycle by stopping the usual drop in progesterone that tells the uterus to shed its lining.
The result is a late period or a missed period for that month. At the same time, stress may change your sleep, appetite, and exercise patterns, which adds further pressure on the cycle.
Stress Vs Pregnancy Vs Hormonal Imbalance
When your period is late, you cannot safely assume that stress affects your menstrual cycle as the only reason. Pregnancy is a very common cause of a missed period in people who have vaginal sex without reliable contraception.
If your period is late and pregnancy is possible, experts advise taking a pregnancy test even if you feel stressed. If the test is negative and the pattern repeats, other causes such as thyroid disease or PCOS can also disturb cycles. These conditions can create stress and hormone imbalance that look similar on the calendar, so you need medical review rather than guessing.
When To Worry About A Missed Or Delayed Period
A small shift of a few days can be normal. You should seek medical advice if your period has been absent for three months in a row and you are not pregnant, or if your cycles suddenly become very irregular after being steady.
Guidelines on amenorrhea note that mental stress is one cause, but they also warn that other medical reasons, such as thyroid problems, high prolactin, or early ovarian failure, need to be ruled out.
Heavy bleeding after a long delay, severe pain, or dizziness also need prompt care. In these cases, stress doesn’t affect your menstrual cycle and it is not safe to treat it as the only reason without a full check.
Emotional Stress And Period Symptoms
You may notice that your mind and your period symptoms seem tied together. Many people report that mood, cramps, sleep, and energy feel worse in stressful months.
Mood Changes And PMS Worsening
During the second half of your cycle, hormone shifts can trigger PMS. You may feel more sensitive, sad, or tense. When life stress is high at the same time, stress affects your menstrual cycle and your brain, so mood swings can feel much stronger.
Some studies suggest that people with PMS may have a different stress hormone response in the luteal phase, which might help explain why small stressors feel bigger before a period, although this research is still developing. This does not mean you are weak. It means your body and brain are reacting to hormone and stress signals together.
Increased Cramping Or Breast Tenderness
Stress can increase muscle tension and change how your brain processes pain. When you are tense, the uterus and pelvic muscles can feel tighter. That can make period cramps feel sharper or longer. Some people also report more breast tenderness when they are under pressure.
Scientific data on this is not as strong as data on ovulation timing, so it is fair to say that evidence is limited. Still, many patients tell their doctors that stress affects their menstrual cycle and makes cramps or breast pain worse, and this matches what is known about stress and pain pathways in general.
Anxiety, Irritability, And Sleep Disruption
High stress often comes with worry, short temper, and poor sleep. At the same time, PMS can cause similar changes. When they happen together, stress affects your menstrual cycle and your daily life.
You may fall asleep late, wake in the night, or notice racing thoughts. Poor sleep then feeds back into higher cortisol the next day, which can keep your cycle disturbed for several months if nothing changes.
Stress-Induced Menstrual Problems
Doctors use the term “abnormal uterine bleeding” for cycles that are too frequent, too far apart, too heavy, or too light compared with normal ranges. Stress is one of several common causes of these stress-induced menstrual problems , along with pregnancy, fibroids, thyroid disease, PCOS, and bleeding disorders.
Irregular Cycles (Long, Short, Or Skipped)
Irregular cycles include those shorter than 21 days, longer than 35 days, or with big swings from one month to the next. Studies in students and working adults show that higher perceived stress often tracks with more irregular cycles, but results are not identical in every group, which means other factors also play a role.
If you see your menstrual cycle lengths jump around during hard times, then calm down again when life settles, stress is a likely factor. If irregularity continues even when stress improves, you need a medical review.
Spotting, Heavy Bleeding, Or Lighter Periods
Some people notice spotting before or between periods during stressful months. Others have very heavy flow after a long gap. A few see very light, short bleeds. All of these can happen when stress affects your menstrual cycle , but they can also signal other conditions such as fibroids, polyps, or pregnancy problems.
Very heavy bleeding, clots larger than a coin, or bleeding that lasts longer than about a week should never be blamed on stress alone. These patterns need a proper exam and sometimes blood tests or scans.
Impact On Perimenopause Or Postpartum Cycles
Perimenopause and the months after birth already involve big hormone swings. During these stages, stress affects your menstrual cycle more easily. People in perimenopause often report irregular timing and changes in flow, and stress can add to hot flashes and sleep problems.
After childbirth, sleep loss, body recovery, and life changes are intense. Breastfeeding itself can delay the return of periods. When stress sits on top of these changes, cycles may stay irregular for longer. Here, too, the research is mostly observational, so doctors are careful not to blame stress for every issue, but it is a real part of the picture.
Stress And Hormone Imbalance
When stress stays high for a long time, it can push many hormones out of balance. In this state, stress and hormone imbalance move together and often shape how stress affects your menstrual cycle . Chronic stress raises cortisol from the HPA axis [hypothalamic pituitary adrenal axis], which can suppress the HPO axis [hypothalamic pituitary ovarian axis] and disturb ovulation signals.
How Cortisol Affects Estrogen And Progesterone
Estrogen and progesterone control most of your cycle changes. Estrogen helps build the lining. Progesterone stabilizes it after ovulation. Together with brain hormones, they keep timing and flow steady.
High cortisol can change how these hormones rise and fall. Human and animal studies show that stress can raise adrenal progesterone and change estradiol [main estrogen] levels at different points in the cycle, although results are not the same in every study. This is one clear way stress affects your menstrual cycle and can trigger stress-induced menstrual problems such as irregular bleeding or stronger PMS.
Over months, these shifts may look like mid-cycle spotting, shorter luteal phases [time after ovulation], or periods that change in flow.
Thyroid Involvement In Stress-Related Cycle Changes
Your thyroid gland in the neck sets your body’s energy speed. Thyroid hormones help control periods, fertility, and pregnancy health. Too little hormone [hypothyroidism] can cause long cycles and heavy bleeding. Too much [hyperthyroidism] can cause light or rare periods.
Some research suggests that chronic stress may affect thyroid function in some people, which then changes the cycle. Evidence is not complete, but several recent studies show that women with menstrual irregularities have a higher rate of undiagnosed thyroid disease.
Gut Health, Blood Sugar, And Inflammation Links
Your gut microbiome [the bacteria in your intestines] helps process estrogen and other hormones. When gut balance is poor, estrogen handling can change, and inflammation can rise. Recent reviews link altered gut bacteria with irregular periods, worse cramps, and perimenopause changes, although many of these studies are still early.
High stress often leads to quick snacks, skipped meals, and high sugar intake. This pattern spikes blood sugar and adds more inflammation. Hospitals and clinics now teach patients that gut problems and poor diet can worsen stress-induced menstrual problems by disturbing hormones and pain signals.
How To Know If Stress Is Affecting Your Cycle
You cannot see hormones, but you can track signs. When stress affects your menstrual cycle , patterns usually appear in both calendar changes and body symptoms.
Warning Signs Of Stress-Related Menstrual Disruption
You should suspect that stress affects your menstrual cycle when changes match clear stressful periods in your life. Examples include cycles that stretch or shrink by more than seven days compared with your usual pattern or a bleed you miss during a tough month, with a normal pregnancy test. Observational work links high psychological stress with more irregular cycles and more frequent anovulation, although it does not prove cause in every case.
If periods settle again when your life becomes calmer, it is quite likely that stress affects period timing for you. If irregularity continues even when you feel stable, another health issue may be present.
Physical And Emotional Symptoms To Track
To see how stress affects your menstrual cycle , keep a simple record. Note start and end of bleeding, flow strength, cramps, headaches, bowel changes, and breast tenderness. Also rate sleep quality, stress level, and mood. Many people notice that emotional stress and period symptoms rise together, especially in the week before bleeding.
What’s Normal Vs What Needs Evaluation
Cycles between 21 and 35 days that stay fairly steady for you are usually considered normal if flow and pain are also in a safe range. A one-time odd month during a known stress spike is common when stress affects your menstrual cycle .
You need medical review if you miss three periods in a row, if cycles become very random for several months, or if flow is much heavier or more painful than before. Serious conditions like thyroid disease, PCOS, fibroids, or early ovarian failure can share signs with stress and hormone imbalance .
How To Manage Stress For A Healthier Cycle
You cannot remove all stress. You can still lower its effect on your body so stress affects your menstrual cycle less over time. Evidence for each method varies, but many are backed by both research and long clinical use.
Lifestyle Strategies (Sleep, Exercise, Nutrition)
Regular sleep keeps cortisol in a healthier rhythm. Disturbed sleep can raise cortisol and change how your brain handles stress. Try to keep the same sleep and wake time most days. This can ease how stress affects period timing and mood.
Moderate physical activity, like walking or light cardio, helps your body clear stress hormones and improves insulin sensitivity. Most guidelines from groups such as WHO and national heart associations support regular movement for hormone and heart health, even though they do not talk only about periods.
Mind-Body Interventions (Breathing, CBT, Journaling)
Mind-body tools target how your nervous system reacts to stress. Slow breathing, muscle relaxation, and short breaks from screens can lower acute cortisol spikes. Reviews of stress programs in women show that these methods can reduce perceived stress and sometimes improve PMS scores, although sample sizes are often small.
Cognitive behavioral therapy [CBT] teaches you to spot and change unhelpful thought patterns. In several studies, CBT reduced anxiety and improved coping in people with chronic health problems, which can lessen how stress affects your menstrual cycle day to day, even if it does not remove all emotional stress .
When To Adjust Contraceptives Or Medications
If you use hormonal birth control, it already shapes your bleeding pattern. Stress can still influence symptoms like spotting, mood, or headaches. If stress and hormone imbalance seem worse after starting a method, consult your doctor.
Doctors may change dose, type, or route, or check for thyroid or other disorders before deciding.
When To See A Doctor About Stress-Related Period Changes
Self-care can help, but some patterns always need medical review, even if you are sure that stress affects your menstrual cycle .
Persistent Irregularities
If your cycles stay irregular for more than three months, or if you are older than 40 and notice sudden strong changes, you should see a doctor. Research on chronic stress shows clear links with ovarian dysfunction, but it also points out that many women with irregular cycles have more than one factor at work.
Severe Pain, Heavy Bleeding, Or Missed Periods
Very strong pain, bleeding that soaks pads or tampons very fast, or long gaps without bleeding can overlap with stress-induced menstrual problems , but they can also signal fibroids, endometriosis, pregnancy problems, or bleeding disorders. You should not assume that stress alone explains such symptoms. Clinical guidelines advise early examination in these situations to prevent anemia and long-term harm.
Recommended Tests & Evaluations
A doctor will ask about your history, stress level, weight changes, medicines, and family health. You may have:
- Blood tests for pregnancy, thyroid, prolactin, and sometimes other hormones.
- Iron tests if bleeding is heavy.
- Pelvic exam or ultrasound to check the uterus and ovaries.
These steps help sort out how stress affects your menstrual cycle and whether another condition also plays a role. Dosage and type of any treatment then depend on your age, diagnosis, and plans for pregnancy, and must be set by a qualified clinician.
FAQ
How Does Stress Affect Your Menstrual Cycle?
Stress affects your menstrual cycle by raising cortisol, which can disturb brain signals to your ovaries. This may delay ovulation, change hormone levels, and trigger irregular bleeding or other stress-induced menstrual problems .
How Does Cortisol Interfere With Reproductive Hormones?
High cortisol can reduce or change the timing of GnRH, LH, and FSH signals from your brain. That disrupts estrogen and progesterone swings, so stress affects your menstrual cycle and can cause clear stress and hormone imbalance .
How Does Stress Change Ovulation, Cycle Length, Or Flow?
When stress affects your menstrual cycle , ovulation may be late or absent. Late ovulation lengthens the cycle. Missed ovulation can lead to skipped periods, light spotting, or, at times, heavier bleeding after a long gap.
Can Stress Increase Cramping Or Breast Tenderness?
Yes, in many people. Stress tightens muscles and can make your brain read pain signals more strongly. As a result, emotional stress and period symptoms like cramps or breast tenderness may feel sharper or last longer.
Can Stress Delay Your Period?
Yes. Stress affects your menstrual cycle by raising cortisol, which may block or delay the LH surge that triggers ovulation. Without on-time ovulation, your period often arrives late or skips that month.
Why Might Periods Come Late During High Stress?
During very stressful weeks, your brain focuses on survival instead of pregnancy. Hormone signals to the ovaries weaken, so stress affects your menstrual cycle by slowing ovulation and making the next bleed show up later than usual.
How Does Stress Contribute To Anxiety, Irritability, Or Sleep Disturbances?
High stress raises cortisol and shifts brain chemicals that control mood and sleep. You may feel anxious, short-tempered, and tired, especially when stress affects period timing and PMS, and both hit at once.
When Should Someone Worry About A Missed Or Delayed Period Due To Stress?
You should see a doctor if a late period repeats for several months, if you miss three periods in a row, or if stress affects your menstrual cycle along with heavy bleeding or severe pain.
What Emotional Symptoms Can Stress Cause Before Or During A Period?
Emotional changes can include worry, sadness, anger, or feeling numb. When emotional stress and period symptoms combine, small problems feel larger, and it may be harder for you to cope with daily tasks.
Does Stress Worsen PMS Or Mood Swings?
Yes, often. When stress affects your menstrual cycle , PMS can start earlier and feel stronger. Mood swings may be sharper, sleep may drop, and you may move from calm to upset much more quickly.










Leave a Comment