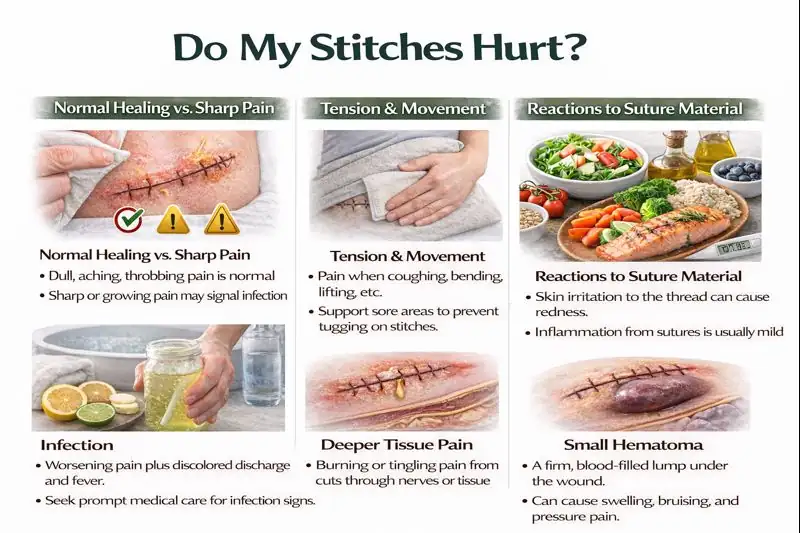
Pain in stitches is common after cuts or surgery. You feel it because your skin, muscles, and nerves are healing from a real injury. Mild pain, slight redness, and a bit of swelling usually come under normal healing, but severe or rising pain can warn you about infection or other problems.
If you have increasing pain, spreading redness, warmth, pus, and fever, you must contact a doctor. When you understand why your stitches hurt and how to control the pain, you can protect the wound and know when to ask for help.
Why Do My Stitches Hurt
Your pain in stitches usually comes from normal healing, pulling on the wound, reactions to the suture thread, or infection. You may also notice pain around surgical stitches , which comes from tissue under and beside the cut, not only the skin line.
Normal Healing Pain Vs Sharp Pain
In the first days, you often feel dull, sore, or throbbing pain in stitches . This happens because tissue is cut, and your body sends blood, immune cells, and repair cells to the area. Normal healing brings mild redness, warmth, and tenderness that peak in the first few days and then slowly fade.
Sharp, stabbing, or burning pain is different. It can come from irritated nerves or an infection. If sharp pain in stitches keeps getting stronger, wakes you from sleep, or makes it hard to move the area at all, that pain pattern is not typical healing, and you should call your doctor.
Tension On The Wound and Movement-Related Pain
Any stretch of the skin can pull on the stitches. Standing up, coughing, laughing, bending, lifting a child, or reaching for a shelf can all tug on the line and give you pain in stitches that feels tight or pulling. Cuts on joints or on the chest and belly often hurt more, because those spots move all day.
Good support helps. Holding a small pillow over your belly stitches when you cough, or using your hand to brace a joint, can lower pulling pain. Simple support like this often helps relieve stitch pain caused by movement.
Inflammation From Suture Material
Your immune system sees the thread as foreign. It reacts with inflammation, which means more blood flow and immune cells in that area. Inflammation (the body’s response that causes redness, warmth, and swelling) can cause mild pain in stitches even when the wound looks clean.
Small red bumps at each stitch hole and slight tenderness often fit normal healing. But if redness spreads out, the skin turns very hot or shiny, or pain rises instead of settling, doctors worry about infection, not just simple inflammation.
Pain From Underlying Tissue Or Nerves
A lot of cuts and operations go deeper than the top skin layer. They may pass through fat, fascia (a tough sheet that wraps muscles), and muscle. Tiny nerves in these layers can stretch, bruise, or get caught in early scar tissue. That can cause shooting, tingling or burning pain in stitches or odd feelings next to the wound.
If you notice numb spots, weakness, or pain that runs down an arm or leg, you should ask your doctor to check for nerve irritation. Early review helps prevent longer nerve problems.
Infection As A Cause Of Increasing Pain
Infections happen when germs get into the wound and start to grow. Large studies on surgical site infections show that growing local pain, warmth, swelling, thicker discharge, and fever are key warning signs.
If pain in stitches gets worse each day, not better, or you see yellow or green pus or a bad smell, or you feel feverish or very tired, you need prompt medical care. That is not when stitch pain is normal for a healing wound.
Small Hematoma Or Swelling Causing Pressure
Sometimes a small pool of blood collects under the skin near the stitches. This is a hematoma (a firm, blood-filled lump under the skin). It can press on tissue and nerves and cause throbbing pain in stitches plus bruising and firmness.
Many small hematomas slowly shrink as your body reabsorbs the blood. But if the lump grows fast, feels very tight, or the skin turns very dark and shiny, a doctor should check it.
How To Relieve Stitch Pain
You can often reduce pain in stitches with simple steps at home, as long as you do not ignore warning signs like pus, fast-spreading redness, or high fever. Good wound care advice begins with clean hands, gentle care, and close watching of the incision.
These methods help you relieve stitch pain while your body repairs the cut.
Cold Packs In The First 48 Hours
In the first one to two days, wrapped cold packs help a lot. Cold makes blood vessels tighten and limits early swelling. Less swelling usually means less pain in stitches .
Place a cold pack or a bag of frozen peas wrapped in a thin cloth over the dressing for short periods. Do not put ice straight on your skin, and do not leave it in place so long that the skin becomes numb or pale.
Warm Compresses After Swelling Subsides
After the early swelling eases, mild warmth often feels better than cold. A warm, clean cloth over the dressing can relax nearby muscles and improve blood flow. That can ease tight, stiff pain in stitches , especially around the belly or back.
Never use strong heat on a very red, hot, or clearly infected area, because heat can increase swelling in an active infection. If you are not sure why the area hurts, ask your doctor before using warmth.
OTC Analgesics And Safe Dosing
Doctors usually suggest paracetamol or sometimes non-steroid anti-inflammatory drugs such as ibuprofen to control pain in stitches for a few days. Research shows that uncontrolled wound pain can raise stress and may even slow healing, so pain relief is not a luxury.
The exact dose and choice of drug vary by age, other illnesses, and the type of surgery. People with kidney, liver, stomach, or bleeding problems need special plans. You should always follow your own doctor’s advice on what to take, how often to take it, and how long to use it for stitch pain after surgery .
Topical Pain Relievers And Dressings
Some doctors suggest numbing gels or creams on the skin around the incision, never deep in the wound. These can soften surface pain in stitches , especially during dressing changes. Only use products your doctor approves, because some creams delay healing or irritate the skin.
Non-stick, soft dressings also protect the area from rubbing and can lower everyday pain around surgical stitches caused by clothing and bedding.
Elevation And Limiting Movement To Reduce Tension
If your wound is on an arm or leg, propping it up on pillows helps fluid drain away and reduces swelling. Less swelling often means less pain in stitches at the end of the day.
Short rest breaks with the limb raised, plus avoiding heavy lifting or sudden twisting, protect the wound edges and keep pain levels down. This kind of care helps shape when stitch pain is normal as healing moves forward.
Gentle Wound Care To Prevent Irritation
Careful cleaning protects the wound and keeps pain in stitches from getting worse. Before you touch the area, you should wash your hands well with soap and water. MedlinePlus advises using normal saline or mild soapy water if your provider has allowed cleaning and avoiding harsh products like alcohol or peroxide that damage tissue.
Pat the skin dry, use fresh dressings as instructed, and never pick at scabs or crusts. Rough handling and scratching increase irritation, raise infection risk, and often turn mild discomfort into severe, longer-lasting pain.
Stitches Pain After Surgery
Many people feel stitches pain after surgery because deeper layers like muscle and fascia, were also cut. Healing in deeper layers takes more time and can cause ongoing pain in stitches , even when the skin looks better on the outside.
Expected Timeline Of Post-Op Stitch Pain
Right after surgery, numbing medicine wears off, and you feel soreness, heaviness, and tightness. This is usually strongest in the first three days. The first seventy-two hours bring the most swelling and tenderness because your body begins the repair process. Pain should slowly ease each day. By the second week, most people feel a clear improvement if the wound is healing normally.
When Pain Should Steadily Improve
With clean wounds, pain in stitches lowers day by day. A steady downward trend is the main sign of healthy healing. If your pain stalls or rises instead of easing, that pattern does not match when stitch pain is normal . Pain that keeps climbing after day three often means irritation, pressure, or early infection.
Activity Restrictions That Reduce Pain
Your surgeon will tell you to avoid lifting, twisting, or bending at first. These limits protect the wound edges. When you follow these instructions, you reduce pulling and cut down on stitch pain after surgery . Moving too early or too fast can stretch the incision and cause bleeding between tissue layers, which increases soreness.
Managing Pain During Wound Stretching
Coughing, sneezing, and rolling in bed make sudden pressure waves in the chest and belly. These can increase pain in stitches for a moment. Many surgeons recommend holding a small pillow on the incision when you cough. This simple support reduces tension on the stitch line. Slow movements and planned posture changes help you stay comfortable.
Scar Formation And Late Tightness Pain
Scars form as collagen (the body’s repair fiber) builds up. In the first month, the scar may feel firm, itchy, or tight. This can cause mild pain around surgical stitches even after the stitches are removed. The American Academy of Dermatology notes that scars soften over time as collagen remodels. If tightness grows instead of fading, your doctor may suggest massage or silicone sheets.
Pain Around Surgical Stitches
It is normal to feel pain around surgical stitches in a wider zone, not only right on the line. This is because inflammation spreads through the nearby tissues as your body works on the injury.
Localized Tenderness Versus Radiating Pain
Localized tenderness stays close to the wound. It hurts when you touch the area but does not spread. Radiating pain travels along a limb or toward the trunk. This type can come from nerve irritation. Radiating discomfort does not always mean damage, but it should be checked if it gets worse or causes numbness.
Skin Sensitivity And Suture Track Irritation
Each stitch hole forms a tiny “track” that can look pink or raised. These tracks sometimes get irritated by friction from clothing or dressings. That irritation can increase pain around surgical stitches , itching, and sensitivity. Wearing loose cotton clothes and using soft dressings can help reduce rubbing.
How Sutures Interact With Nearby Nerves
Stitch material may sit close to small nerves. Swelling pushes on these nerves and can cause tingling, buzzing, or sharp pain in stitches . After swelling drops, these sensations usually fade. If you notice sudden weakness or ongoing numbness, medical review is needed.
When Adjacent Tissue Causes Discomfort
Muscles and fascia next to the wound also heal. If these layers are tight, they can create deeper aching. Movements like standing or reaching may cause pulling. This deeper pain often improves as the tissue regains strength and flexibility.
When Stitches’ Pain Is Normal
You can feel more confident when you know when stitch pain is normal . Normal pain follows a clear pattern: steady improvement, mild soreness, and no spreading redness.
Mild Soreness, Redness, and Firmness
A healing wound always has some color change. Mild redness and warmth near the incision are normal healing and usually go along with gentle pain in stitches . The area might feel firm because your body is building new tissue.
Typical Pain Pattern Over Days 1 to 14
In the first days, soreness is stronger. By day five, most people feel less tightness. By day ten, swelling and tenderness continue to drop. This timeline describes when stitch pain is normal and what most doctors expect.
Acceptable Swelling And Bruising
Small patches of bruising under the skin are common. These bruises slowly fade without treatment. Mild swelling that stays near the wound is also normal. Rapid swelling or swelling that spreads up or down the limb is not typical and needs medical attention.
How To Track Improvement Day By Day
Many doctors recommend writing a simple daily pain score. This helps you see if the pain in stitches is moving downward. Keeping track also helps your doctor understand your healing pattern.
Signs Of Infected Or Problematic Stitches
Infection is the most serious reason for rising pain. Here are the key signs that come from surgical infection.
Increasing Redness, Warmth, Spreading Pain
If redness spreads outward in a wider circle or the skin feels hot, swelling is growing, and pain in stitches gets worse, infection becomes likely. This needs prompt care.
Pus, Foul Drainage, or Fever
Thick yellow or green drainage, a bad smell, or fever strongly suggest infection. These symptoms, paired with pain around surgical stitches , mean the wound must be checked quickly.
Wound Edges Separating Or Excessive Bleeding
If the wound pulls open or bleeds steadily through dressings, the stitches may not be holding. This is not when stitch pain is normal and requires urgent medical help.
Severe Throbbing Pain Not Helped By Meds
If approved medicine no longer helps and you feel strong throbbing or pressure, there may be a deeper problem like fluid buildup or infection.
Practical Wound Care Steps To Reduce Pain
Good wound care protects healing tissue and reduces pain in stitches every day.
Cleaning, Drying And Correct Dressing Changes
Doctors usually suggest gentle cleaning with saline or mild soapy water if allowed. Pat dry and cover with a fresh dressing. Clean hands and clean supplies lower infection risk.
Avoiding Soaking
You should avoid baths, swimming, and hot tubs because soaking softens the skin and lets germs enter. Showers are often allowed if your doctor approves.
Keeping Sutures Protected During Activity
Loose clothing, soft fabric, and careful movement reduce friction and help relieve stitch pain caused by rubbing.
When And How To Remove Sutures Safely
Only trained professionals should remove stitches unless your doctor gives clear instructions. Early removal or forceful pulling can reopen the wound and increase pain in stitches .
Pain Control: Medications and Non-Drug Options
Good pain control keeps you mobile and helps with healing.
Acetaminophen Versus NSAIDs
Doctors choose medicine based on your age and health. Acetaminophen lowers pain without affecting bleeding. NSAIDs help with swelling but are not right for everyone. They are used with caution after some operations. Use only what your doctor approves to manage stitch pain after surgery .
Topical Anesthetics
Mild numbing products may help with dressing changes. Only use them on intact skin and only if your doctor agrees.
Nonpharmacologic Pain Relief
Resting the limb, using soft pillows, and slow breathing can lower pain in stitches by relaxing the area. Gentle posture changes protect the wound from tension.
When Prescription Analgesics Are Appropriate
For major surgery, doctors may prescribe stronger short-term pain medicine. These medicines are used only as needed and stopped when the pain becomes mild.
Preventing Stitch Pain and Re-Injury
Avoiding extra strain protects scar formation.
Wound Support During Movement
Light taping or soft compression wraps, if approved, help reduce pulling and lower pain around surgical stitches .
Stepwise Return To Activity
Increase activity slowly. If a movement increases pain in stitches , reduce or pause it.
Protective Clothing And Padding Over Sutures
Soft pads prevent rubbing from waistbands or straps and help you relieve stitch pain during daily tasks.
When To Seek Emergency Attention
Certain signs require fast help.
High Fever, Spreading Redness, Severe Bleeding
These signs point to infection or active bleeding and must be checked immediately.
Signs Of Sepsis
A fast heartbeat, chills, dizziness, and confusion, along with severe pain in stitches, can signal a dangerous response to infection.
Loss Of Limb Function Or Uncontrollable Pain
Sudden weakness or pain so strong that you cannot move safely needs urgent evaluation.
FAQs
How long should stitches hurt?
Normal pain in stitches usually improves within one to two weeks. The pain should keep moving downward. If swelling or redness rises instead of settling, you should call your doctor for guidance.
When should I contact my doctor?
Call your doctor if pain around surgical stitches gets worse, if redness spreads, or if drainage changes color. Sudden fever or strong pressure pain are also important reasons to seek help.
Can I apply ointment or antibiotic cream?
Use the ointment only if your doctor says it is safe. Some wounds heal better when kept dry. If you add products without advice, you can irritate the skin and cause pain in stitches .
Are hot showers or baths safe?
Showers are often allowed if you protect the wound. Baths and pools are not safe until the area is sealed because soaking can raise stitches pain after surgery and infection risk.
Will the stitches make a scar and can pain predict scarring?
Scars form in every stitched wound. Pain level does not predict scar size. Good wound care lowers irritation, reduces friction, and can decrease pain in stitches during healing.
Is it safe to take ibuprofen after surgery?
Doctors approve ibuprofen in some cases but avoid it in others. Its use depends on the type of surgery and your health. Always ask before using it for stitches, or pain after surgery .
Can tight clothing cause stitch pain?
Yes, tight fabrics press on the wound and increase pain in stitches . Soft, loose clothing prevents rubbing and keeps the area comfortable while healing.
What should I do if stitches start to pull out?
If a stitch loosens or lifts, cover the spot and avoid touching it. Contact your doctor quickly because loose stitches can increase pain around surgical stitches and raise infection risk.














Leave a Comment