Childhood obesity is one of the most serious health concerns today. It affects children physically, emotionally, and socially. Parents often wonder, what is childhood obesity and how can they recognize it early? The truth is, obesity is not only about appearance. It involves complex factors such as genetics, food choices, screen time, and even social conditions.
Understanding the childhood obesity definition, its symptoms, causes, and effective prevention can help families take the right steps toward long-term health.
Overview
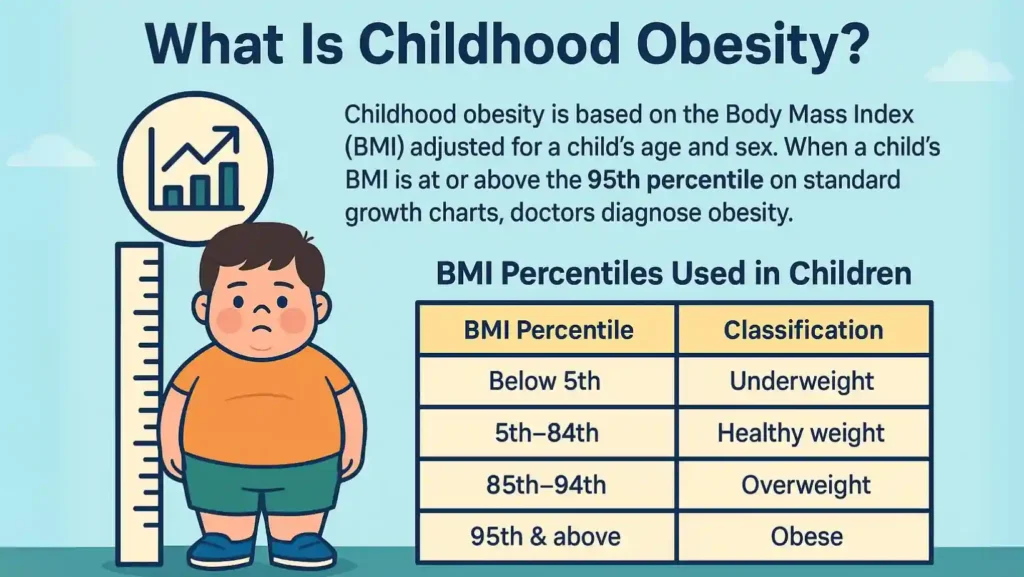
What Is Childhood Obesity?

Childhood obesity is based on the Body Mass Index (BMI) adjusted for a child’s age and sex. When a child’s BMI is at or above the 95th percentile on standard growth charts, doctors diagnose obesity. Unlike adults, children are still developing, so growth comparisons are the most reliable way to identify excess weight.
BMI Percentiles Used in Children:
| BMI Percentile | Classification |
| Below 5th | Underweight |
| 5th–84th | Healthy weight |
| 85th–94th | Overweight |
| 95th & above | Obese |
How Common Is Childhood Obesity?
The rates of pediatric obesity are rising worldwide. In the U.S., about 1 in 5 children and adolescents are obese. The World Health Organization estimates over 340 million children globally face childhood overweight issues. Alarmingly, obesity in early childhood often continues into adulthood, raising risks of heart disease, diabetes, and mental health concerns.
Symptoms And Causes
What Are The Symptoms Of Childhood Obesity?
Childhood obesity symptoms can show up in both the body and behavior. Parents may notice:
- Clothes fitting tighter than expected for age
- Shortness of breath or tiring quickly during play
- Snoring or pauses in breathing (possible obstructive sleep apnea)
- Joint pain / Blount’s disease causing difficulty in movement
- Dark, thick skin patches (a sign of insulin resistance)
- Low confidence, withdrawal from peers, or signs of depression
What Causes Childhood Obesity?
There is no single cause. Multiple overlapping triggers explain why children gain unhealthy weight.
Genetics And Epigenetics
A family history of obesity raises risk. Genetics influence how bodies store fat and burn calories. Epigenetics, or changes in gene activity without altering DNA, can also affect metabolism. For example, maternal pre-pregnancy obesity or gestational diabetes can predispose children to extra weight even before birth.
Family And Home Environment Factors
Daily habits in the home strongly influence weight. Easy access to fast foods, sugary drinks, and snacks often leads to unhealthy eating habits in children. Lack of structured family meals, late-night eating, and limited exposure to vegetables worsen the problem. Parents’ activity levels matter too. If adults are sedentary, children often mirror these habits.
Social Determinants Of Health
Social determinants of health (SDoH)—like safe neighborhoods, access to healthy food, and school resources—play a major role. Children in low-income families often lack parks for active play and may rely on processed foods because they are cheaper.
Cultural Factors
Cultural factors (advertising, marketing) also push kids toward poor choices. Junk food ads, cartoon packaging, and fast-food sponsorships in schools make high-calorie foods appealing. Junk food and childhood obesity are closely linked in many studies.
Other Health Conditions
Some kids gain weight due to underlying medical problems. Hormonal imbalances (hypothyroidism, GH deficiency, Cushing syndrome) slow metabolism. Rare genetic syndromes (Prader-Willi, Bardet-Biedl, Alstrom, leptin deficiency, PCSK1) cause uncontrollable appetite. Certain medications (antipsychotics, corticosteroids) also increase appetite.
What Are The Effects Of Childhood Obesity?
Physical Complications
The effects of childhood obesity are far-reaching. Extra weight increases risk for:
- Diabetes (type 2, even in young children)
- High blood pressure and abnormal cholesterol (Complications: hypertension, dyslipidemia)
- Fatty liver disease
- Asthma and breathing issues
- Heart disease risk in adolescence
- Joint pain that limits activity
Emotional And Social Effects
Children often face bullying / social isolation / low self-esteem. The stigma of obesity can lead to withdrawal and depression. These emotional wounds may last longer than physical ones.
Diagnosis And Tests
How Is Childhood Obesity Diagnosed?
Doctors use childhood BMI calculations alongside growth charts from the CDC (Centers for Disease Control and Prevention) to classify weight. They consider age, sex, and growth trends. BMI above the 95th percentile confirms obesity.
Doctors may also check for related childhood lifestyle diseases such as diabetes, high cholesterol, or liver issues. Sleep studies may be done if there are signs of apnea. A full assessment helps distinguish obesity from temporary weight gain during growth spurts.
Management And Treatment
What Is The Treatment For Childhood Obesity?
Lifestyle Changes (Diet, Activity, Screen Time)
The foundation of childhood obesity treatment lies in gradual lifestyle changes:
- Replacing sugary drinks with water or milk
- Reducing processed foods and encouraging fruits, vegetables, and whole grains (childhood nutrition and weight management)
- Increasing daily activity with outdoor play
- Reducing screen time / sedentary behavior and promoting physical hobbies
- Ensuring proper sleep, as poor sleep patterns affect hormones that regulate hunger
Professional Treatment Options
When lifestyle changes aren’t enough, professional care is needed. Options include:
- IHBLT (Intensive Health Behavior & Lifestyle Treatment): Structured programs led by dietitians, counselors, and doctors.
- Pediatricians: Provide monitoring and guidance on growth and development.
- Psychologists / Psychiatrists: Address eating behaviors, depression, or anxiety.
- Bariatric / Metabolic Surgery: Considered only for adolescents with severe obesity and major complications, after all other approaches fail.
Prevention

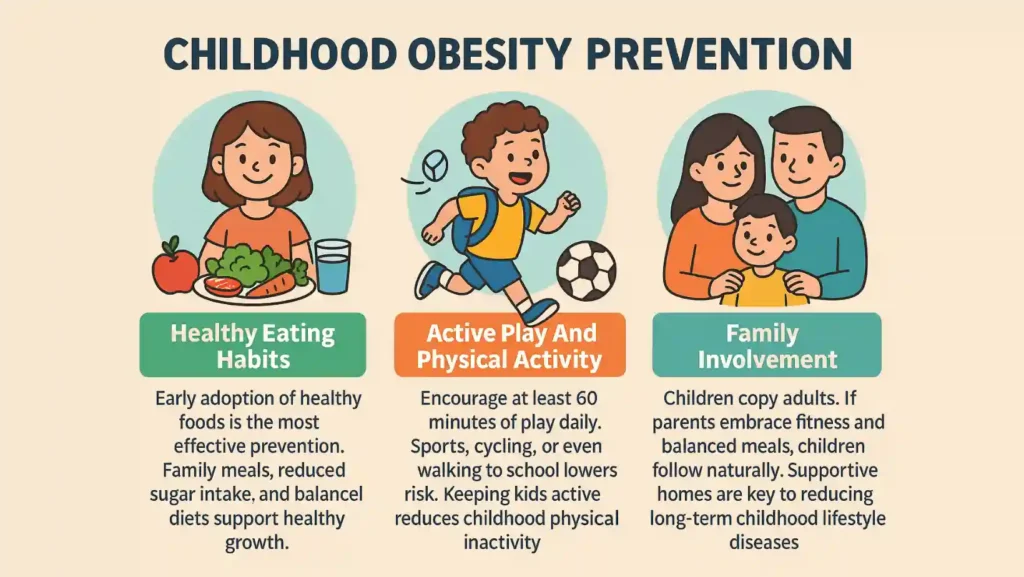
Childhood Obesity Prevention Strategies
Healthy Eating Habits
Early adoption of healthy foods is the most effective prevention. Family meals, reduced sugar intake, and balanced diets support healthy growth.
Active Play And Physical Activity
Encourage at least 60 minutes of play daily. Sports, cycling, or even walking to school lowers risk. Keeping kids active reduces childhood physical inactivity.
Family Involvement
Children copy adults. If parents embrace fitness and balanced meals, children follow naturally. Supportive homes are key to reducing long-term childhood lifestyle diseases
Living With
How Can I Help My Child With Obesity?
Parents should avoid blame. Instead, focus on small, achievable changes. Praise effort rather than numbers on the scale. Work closely with healthcare providers to design a personalized plan.
Childhood Obesity And Diabetes: What Parents Should Know?
Childhood obesity and diabetes often go hand in hand. Excess fat lowers insulin sensitivity, leading to type 2 diabetes. Regular screenings and early treatment can prevent complications like kidney disease and nerve damage later in life.
The Bottom Line
Childhood obesity is more than just “baby fat.” It is a medical condition with serious physical and emotional consequences. While causes are complex, prevention and management are possible through family involvement, healthy eating, physical activity, and medical guidance. The earlier families act, the better the outcomes. Every small change in daily routine can protect a child’s future health.
FAQs
What is childhood obesity?
It is when a child’s BMI is at or above the 95th percentile for age and sex on CDC growth charts. Doctors use this measure to identify excess weight in children.
What are the 4 types of obesity?
The main categories are genetic obesity, hormonal obesity, obesity from environment and lifestyle, and obesity caused by medications or other health-related conditions.
What are the 6 C’s of childhood obesity?
They include cell (biology), child (behavior), clan (family), community, country (policy), and culture. Together, they explain how weight gain develops in children.
What is the best treatment for obesity?
The best treatment combines healthy eating, physical activity, and behavior therapy. For some adolescents, medical programs or surgery may be considered under strict medical guidance.
What are the 5 main causes of obesity?
Genetics, poor diet, low physical activity, lack of proper sleep, and certain medications are the five leading causes that contribute to obesity in children.
What is the root of childhood obesity?
There is no single root cause. It results from a mix of genetic factors, unhealthy eating patterns, social influences, and environmental barriers to healthy living.
Who is responsible for childhood obesity?
Responsibility is shared among families, schools, food industries, and healthcare providers. Parents play the most direct role, but wider community and policy support are also critical.













Leave a Comment