Obesity and genetics are tied in more ways than people think. Extra weight does not only come from overeating or lack of exercise. For some, the body is wired by genes to hold fat more easily. This explains why two people can eat the same meals and stay active but gain weight differently.
Understanding this link matters because it changes how doctors look at weight problems. Some forms of obesity respond well to lifestyle changes. Others need medical testing or treatment. Let’s break down how genes and environment interact, what makes obesity run in families, and how children may inherit risks.
Is Obesity Genetic?
The question is obesity genetic has been studied for decades. The answer is yes, but not always in the same way. Some people inherit single faulty genes that strongly influence hunger, metabolism, or fat storage. Others carry dozens of small changes across the genome that, combined, increase the risk of weight gain.
Still, lifestyle, sleep, diet, and stress remain critical. Genes create the base risk, while environment decides how strongly those genes act.
Hereditary Obesity Explained
Hereditary obesity refers to weight problems passed down through genes. This does not mean every child of overweight parents will be obese. It means certain genetic variants raise the odds.
Researchers study whether is obesity hereditary by looking at twins and families. Identical twins, even when raised apart, often show similar weight patterns. That proves a genetic factor exists.
Family History And Obesity: How Strong Is The Link?
Family history and obesity have a clear relationship. Children of two obese parents face up to an 80 percent higher risk of becoming obese compared to those with lean parents. But family ties also mean shared food, routines, and cultural habits. So, the link is both genetic and environmental.
Genetic Obesity Vs. Lifestyle Causes
When weight gain stems mostly from genes, it is called genetic obesity. But many people are obese due to lifestyle causes such as high-calorie food, stress eating, or less movement.
Scientists use the term lifestyle and genetics obesity to stress that both matter. For most people, lifestyle factors dominate, but genes explain why some gain weight faster or struggle more to lose it.
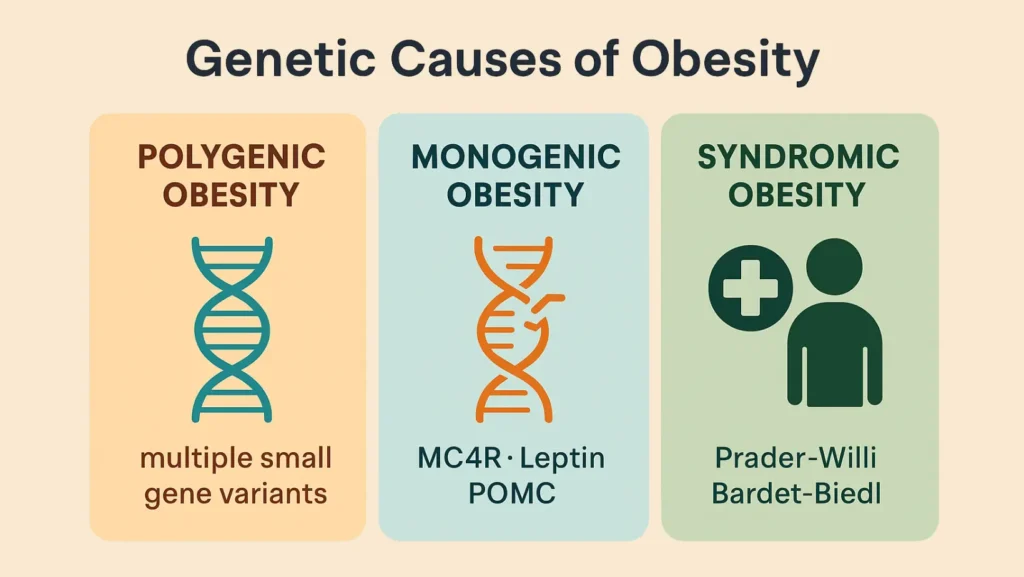
Genetic Causes Of Obesity: Polygenic, Monogenic, And Syndromic Causes
Scientists group genetic causes of obesity into three categories: polygenic, monogenic, and syndromic.
Polygenic Obesity: How Multiple Genes Contribute To Weight Gain
Polygenic obesity happens when many genes together create higher risk. Each gene may add only a small effect. But in combination, they influence hunger, satiety, and fat storage.
One well-studied example is the FTO gene (fat mass and obesity-associated). Variants in this gene make people hungrier and more likely to snack. Over time, this leads to higher body fat.
Other obesity susceptibility genes include those affecting energy use, insulin response, and how fat cells grow. Studies called Genome-wide association studies (GWAS) identify hundreds of such genes.
The Role Of FTO In Obesity
The FTO gene (fat mass and obesity-associated) is the strongest known gene linked to obesity. People with risky versions tend to eat more and crave calorie-dense food. This does not mean obesity is unavoidable, but it raises the chance.
Monogenic Obesity: Severe Obesity Caused By A Single Gene
Monogenic obesity is rare but severe. Here, one gene mutation drives massive weight gain, often starting in childhood.
Examples include:
- MC4R deficiency (Melanocortin-4 receptor): disrupts brain appetite control.
- Leptin deficiency: prevents the brain from sensing fullness.
- POMC deficiency (Proopiomelanocortin) or PC1/3 deficiency (Prohormone convertase 1/3): both alter hunger regulation.
These conditions often require medical testing and sometimes hormone therapy.
Syndromic Obesity: The Links Between Genetic Syndromes And Obesity
Some syndromes involve obesity as part of a larger set of problems. These are called syndromic obesity cases. They usually include intellectual or developmental delays, vision problems, or organ issues.
Examples of genetic obesity syndromes:
- Prader–Willi syndrome: causes insatiable hunger.
- Bardet–Biedl syndrome: includes obesity, kidney disease, and vision loss.
- Cohen syndrome: leads to weight gain plus developmental problems.
- Fragile X syndrome: sometimes linked to obesity risk.
These conditions highlight how complex the genetic contribution can be.
Childhood Obesity And Genetic Factors
Childhood obesity and genetic factors are closely tied. Early weight gain often hints at strong genetic influence.
How Family Genetics Shape Childhood Obesity Risk
Genes passed from parents can strongly impact children’s metabolism. A child’s environment adds to this. For example, a home filled with processed food and little outdoor activity magnifies genetic risk.
Genetic Factors That Cause Obesity In Kids
Several genetic factors that cause obesity in children are well known:
- Leptin deficiency makes kids feel hungry all the time.
- POMC deficiency affects hormone balance, leading to rapid weight gain.
- MC4R deficiency disrupts brain hunger signals.
Doctors sometimes run tests for childhood obesity genetics when weight gain is extreme or starts very early.
Emerging Studies: Epigenetics And Obesity
Modern research shows genes are not the only story. Epigenetics studies how lifestyle influences gene activity.
How Genes And Environment Interact
Food, sleep, exercise, and stress all affect gene function. For example, a child exposed to poor diet during pregnancy may develop higher risk of obesity. These changes in obesity epigenetics do not alter DNA itself, but they change how genes work.
Can Genetic Obesity Be Prevented?
While no one can change their DNA, people can lower risk by focusing on environmental factors (diet, exercise, stress). Regular activity, balanced meals, and good sleep can limit how strongly obesity genes express themselves.
This prevention is also important for conditions linked to obesity, such as Metabolic dysfunction-associated steatotic liver disease (MASLD).
Are Your Genes Your Destiny?
People often fear their genes seal their fate. The truth is genes load the gun, but lifestyle pulls the trigger.
Environmental Factors Vs. Genetic Predisposition
Even with high genetic risk, the environment plays a key role. Two siblings with the same genes can have very different outcomes if one eats healthy and exercises while the other lives sedentary.
This balance is why genetics and obesity are studied alongside diet, stress, and social factors.
The Health Crisis Of Digital And AI Natives: Childhood Obesity In Gen Alpha And Gen Beta
Today’s kids, known as Gen Alpha and Gen Beta, grow up with devices. Constant screens mean less movement and more snack consumption. That fuels obesity in young people who already carry risky genes.
Experts warn that without action, childhood obesity genetics combined with digital lifestyles could create a major health crisis in the future.
The Bottom Line
Genetic causes of obesity explain why weight gain differs from person to person. Some face high risk due to genes like FTO, MC4R, or leptin pathways. Others may develop obesity through shared family habits.
Still, lifestyle changes matter. Knowing your family history and obesity risk is useful, but eating balanced meals, exercising, and managing stress can offset much of the danger. For severe genetic forms, medical help is key.
Genes are not destiny. They are risk markers. And risk can be managed.
FAQs
What is the link between obesity and genetics?
Obesity and genetics connect through hunger, metabolism, and fat storage. Genes raise risk, but lifestyle factors decide how strongly those genes act.
What is true regarding the genetics of obesity?
Obesity can be polygenic, monogenic, or syndromic. Multiple genes or single mutations both contribute. Genes set the base risk while habits shape the outcome.
Is obesity inherited from mother or father?
Both parents contribute risk. Genetic influence comes from both sides, though maternal environment during pregnancy can add epigenetic effects.
Does obesity affect DNA?
Obesity does not change DNA code but it can alter epigenetic markers. These changes switch genes on or off, influencing metabolism and future health.
What is the main cause of obesity?
Most cases result from lifestyle factors such as diet and low activity. Genetic predisposition makes some people more vulnerable but daily choices matter greatly.
Can genetic obesity be cured?
There is no cure for genetic obesity. Some rare forms can be treated with hormone therapy or targeted care. Lifestyle changes still help manage weight.
Why do genetics cause obesity?
Genetics cause obesity by disrupting appetite, fullness, and fat storage. Faulty leptin, MC4R, or POMC pathways raise hunger and energy imbalance, leading to faster weight gain.












Leave a Comment