Understanding Urinary Tract Infections (UTIs)
What is a Urinary Tract Infection?
A urinary tract infection is one of the most common bacterial infections affecting patients of all ages. Urinary tract infection refers to an infection that can develop in any segment of the urinary system, which encompasses the kidneys, bladder, ureters, or urethra.
Bacteria, usually E. coli, cause most cases. While it can affect anyone, women are particularly susceptible due to their shorter urethra, which allows bacteria to reach the bladder more easily.
A 25-year-old woman visiting the emergency room with burning urination and cloudy urine often receives an immediate urine test. The results confirm the presence of bacteria and white blood cells, pointing to UTI.
Causes of Urinary Tract Infections
The causes of urinary tract infection, it is important to remember that infections are often linked to lifestyle, health conditions, and hygiene. Main causes include:
- Bacteria spreading from the bowel into the urinary tract
- Poor personal hygiene after using the toilet
- Sexual activity without proper hygiene
- Holding urine for too long, which allows bacterial growth
- Use of catheters in hospitalized patients
- Dehydration that reduces flushing of bacteria
- Weakened immune system from diseases like diabetes
For instance, diabetic patients face a higher risk of recurrent UTIs because their urine may contain more glucose, which bacteria thrive on.
Symptoms of Urinary Tract Infections

Urinary tract infection symptoms usually start mild but can progress quickly. Patients often report:
- Painful urination with a burning sensation
- Patients may experience a strong urge to urinate but only pass small quantities of urine.
- Blood-tinged or cloudy urine
- Pelvic discomfort in women and rectal discomfort in men
- Foul urine odor
- Fatigue and low-grade fever
If left untreated, symptoms may worsen, leading to back pain, high fever, and nausea. These signs may indicate kidney involvement, which requires urgent treatment.
Risk Factors for Developing UTIs
Certain groups are more vulnerable. Important risk factors include:
- Being female
- Menopause due to hormonal changes
- Pregnancy, where the uterus presses against the bladder
- Diabetes or other chronic diseases
- Frequent use of urinary catheters
- Low fluid intake and poor hydration habits
In elderly patients, confusion and sudden behavior changes may be the only visible symptom of UTI, which highlights the importance of thorough assessment.
Nursing Diagnosis for Urinary Tract Infection
NANDA Nursing Diagnosis for UTI
A NANDA nursing diagnosis for UTI helps nurses identify specific patient needs. Examples include:
- Acute pain related to bladder inflammation
- Impaired urinary elimination due to infection and urgency
- There is a potential risk of sepsis if bacteria disseminate into the bloodstream.
- Knowledge deficit about hygiene and hydration for prevention
Common Nursing Diagnosis Examples for UTIs
Some practical nursing diagnoses associated with urinary tract infections include:
- Pain management nursing diagnosis for patients reporting burning urination
- Urinary elimination problems nursing care when patients struggle with urgency and frequency
- Risk of infection care plan for hospitalized patients with catheter use
Example: A catheterized patient in intensive care has a nursing diagnosis of “risk for infection” because bacteria can enter through the catheter if proper care is not maintained.
Nursing Care Plan for UTI Patients
An effective nursing care plan for UTI must include:
- Symptom assessment and pain management
- Encouragement of hydration to improve fluid balance in nursing
- Administration of antibiotics as prescribed with proper antibiotic education for patients
- Hygiene education including correct wiping and urination after sexual activity
- Continuous monitoring for fever, chills, or worsening pain
Such structured planning ensures patient comfort, reduces recurrence, and prevents complications.
Nursing Assessment for UTI
Thorough Patient Assessment
Assessment involves direct observation and patient communication. Nurses typically look for signs such as burning sensation during urination, frequent bathroom visits, cloudy urine, or fever.
Gathering Patient History and Symptoms
History includes questions about fluid intake, hygiene habits, sexual activity, prior UTIs, and use of catheters. In recurrent UTI in nursing assessment, documenting frequency helps doctors choose preventive antibiotics.
Utilizing Laboratory Tests for Diagnosis
Lab confirmation is critical. Urinalysis shows the presence of white blood cells, blood, and bacteria. Culture tests identify specific organisms, guiding targeted urinary tract infection medication choices.
Nursing Care Strategies for UTI Management
Medication Administration for UTI Treatment
Urinary tract infection treatments usually include antibiotics like nitrofurantoin or trimethoprim-sulfamethoxazole. Nurses stress completing the entire course of drugs. Skipping doses increases resistance. This highlights the necessity of providing antibiotic education to patients.
Promoting Proper Hydration
Adequate hydration flushes out bacteria. Nurses encourage patients to drink at least 8 glasses of water daily. Monitoring both intake and output is vital for ensuring fluid balance in nursing practice. Good hydration also supports hydration and UTI prevention.
Emphasizing Good Hygiene Practices
Proper hygiene practices include wiping front to back, avoiding harsh soaps, wearing cotton underwear, and emptying the bladder soon after sexual activity. These are key bladder health nursing interventions that reduce infection chances.
Patient Education and Lifestyle Guidance
Lifestyle guidance involves stress on hydration, diet, and preventive steps. Cranberry juice, although debated, is sometimes recommended as an additional preventive measure.
UTI Complications and Nursing Interventions
Potential Complications of Untreated UTIs
If untreated, UTIs may progress to:
- Pyelonephritis (kidney infection)
- Sepsis
- Permanent kidney damage
- Recurrent infections that reduce quality of life
Nursing Interventions for UTI Care
Nurses provide interventions such as:
- Monitoring urine color and volume
- Ensuring timely pain relief
- Teaching patients about prevention strategies
- Administering correct urinary tract infection medication
- Addressing emotional support and reassurance
Patient Education and Follow-Up Care
Patients are advised to seek follow-up care within 2–3 days if symptoms do not improve. Nurses stress returning immediately if fever, flank pain, or blood in urine appear.
Urinary Tract Infection Treatments and Medications
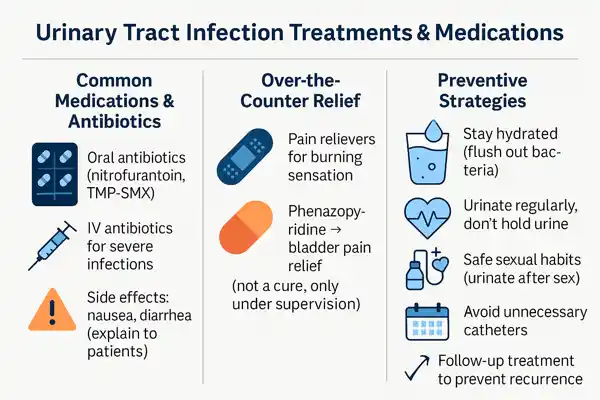
Common UTI Medications and Antibiotics
Urinary tract infection medication often includes oral antibiotics. Severe infections may require intravenous drugs. Side effects like nausea and diarrhea must be explained clearly to patients.
Over-the-Counter Relief Options
OTC pain relievers reduce burning sensations. Phenazopyridine offers bladder pain relief but does not cure the infection. Nurses advise using it only under supervision.
Preventive Strategies to Reduce Recurrence
Prevention strategies include:
- Staying hydrated
- Urinating regularly
- Practicing safe sexual habits
- Avoiding unnecessary catheter use
- Following up on treatment
Cultural Considerations in UTI Nursing Care
The Importance of Cultural Competency in Nursing
Patients may view infection differently depending on cultural beliefs. For example, some communities may use herbal remedies before seeking antibiotics. Nurses must listen and guide without dismissing these practices.
Effective Communication in Cultural Context
Using simple words and clear explanations improves compliance. In multicultural settings, providing education in the patient’s native language supports better understanding.
Respecting Privacy and Cultural Norms
Since urinary issues are sensitive, maintaining privacy is essential. Female patients in conservative cultures may prefer same-gender providers for intimate care. Respecting this improves trust.
Final Thoughts on Nursing Diagnosis for UTI
Building a nursing diagnosis for UTI means addressing both medical and emotional needs of the patient. Nurses should focus on infection control, hydration, pain relief, and lifestyle changes.
A structured nursing care plan for UTI is the best way to manage symptoms, avoid kidney complications, and reduce recurrence. Patient education remains the cornerstone of long-term prevention.
FAQs
What are nursing interventions for UTI?
Nursing interventions include administering antibiotics, supporting hydration, teaching hygiene, reducing pain, monitoring symptoms, and encouraging follow-up appointments for continued care and infection prevention.
What are interventions for patients with UTI?
For patients, interventions include pain management, hydration, regular urine checks, antibiotic teaching, lifestyle education, and reassurance. These steps improve recovery and prevent repeated infections.
What are the top 3 nursing diagnoses?
The top three nursing diagnoses for UTI are acute pain related to burning urination, impaired urinary elimination linked to urgency and frequency, and risk of infection complications.
What is the diagnosis for urinary tract infection?
The diagnosis is confirmed using patient history, urine analysis, culture, and observation of urinary tract infection symptoms. These findings help decide the correct treatment and medications for recovery.
What are the nursing interventions for infection?
Nursing interventions include antibiotic administration, fever monitoring, patient education on prevention, maintaining hydration, and observation for complications. These are vital steps to ensure quick and complete recovery.
What are the five nursing interventions?
Five nursing interventions are pain control, hydration support, monitoring infection progression, hygiene teaching, and emotional support. These interventions ensure holistic care for patients with UTIs.
What is the priority of care for a UTI?
The priority of care is symptom relief, infection control with correct urinary tract infection treatments, hydration improvement, and education to prevent recurrence, ensuring the patient avoids further complications.









Leave a Comment