Antibiotics can make you tired, and it happens to many people. You may feel unusual fatigue (deep tiredness) or low energy while on antibiotics. This happens because the medicine not only fights infection but also affects gut bacteria, nutrient levels, and your immune system’s balance.
While this tiredness is usually temporary, understanding why it happens can help you manage it better and recover faster.
Why You Might Feel Tired While Taking Antibiotics
Feeling tired while on antibiotics is common. When you’re sick, your immune system works hard to destroy harmful bacteria. This fight itself consumes a lot of your body’s energy. Antibiotics, while helping you recover, can add stress to your system.
Some antibiotics affect your liver or kidneys, which must work extra hard to process the drug and remove toxins. That process can make you feel sluggish and weak.
Another reason antibiotics make you tired is that they can upset your gut health. Since about 70% of your immune system is in your gut, any imbalance there can affect your overall energy and mood. When antibiotics kill off good bacteria, it can cause bloating, poor digestion, and fatigue.
Is Fatigue A Normal Response Or A Side Effect?
Fatigue from illness is normal; your body is busy healing. But sometimes antibiotics add an extra burden. A fatigue side effect means the medicine itself is causing tiredness, beyond what your infection would cause. You may see new sleepiness or weakness after starting the drug. That hints that fatigue is a side effect, not just illness.
How Soon After Starting Antibiotics Fatigue Can Begin
For some, tiredness begins within hours of the first dose. For others, it takes a few days. If your energy levels drop noticeably soon after starting your medication, the antibiotic is likely playing a role.
Sometimes fatigue worsens midway through treatment as gut imbalance increases. In rare cases, you might feel most tired near the end of your course or even a few days after stopping it, as your body rebalances itself.
How Antibiotics Affect Your Body’s Energy Levels
The Connection Between Antibiotics And Gut Health
Your intestines host helpful bacteria. They help you digest food and produce vitamins. Antibiotics kill many bacteria, including helpful ones. That imbalance is called gut dysbiosis (bad gut mix). When helpful bacteria decline, digestion can slow, and nutrient use drops. That leads to fatigue.
How Gut Imbalance Can Lead To Tiredness
If antibiotics kill too many good bacteria, your digestion slows. You may absorb fewer nutrients, especially iron and vitamin B12, which are key for energy. This is another clear way antibiotics make you tired and weak . Poor digestion also means your body spends more effort breaking down food, leaving less energy for you.
Impact On Metabolism And Nutrient Absorption
Your metabolism is how your body makes and uses energy. When antibiotic-driven changes alter digestion, your metabolism can slow. You might burn energy less efficiently. When nutrients are not absorbed fully, your cells run out of fuel. That drains you.
The Science Behind Antibiotic-Induced Fatigue
How Antibiotics Interact With Body Systems
Antibiotics circulate through your bloodstream and affect multiple organs. Some pass through the brain and influence neurotransmitters (chemical messengers). That can cause sleepiness or dizziness. Others affect nerve signals or muscle function, which adds to the feeling of weakness. The reason why antibiotics make you tired is this broad, system-wide impact.
The Role Of The Immune Response In Feeling Drained
When bacteria die, your body must clean up their remains. That triggers inflammation. Inflammation releases signaling molecules (cytokines) that tell your body to slow down and rest. This immune response often leads to deep fatigue.
Why Some Antibiotics Trigger More Fatigue Than Others
Some antibiotics, like fluoroquinolones, can affect mitochondria (the energy-producing parts of your cells). When mitochondria slow down, you feel physically tired. Others may upset the stomach or cause dehydration, both of which add to fatigue. That’s why antibiotic tiredness varies from person to person.
Common Antibiotics Known To Cause Tiredness
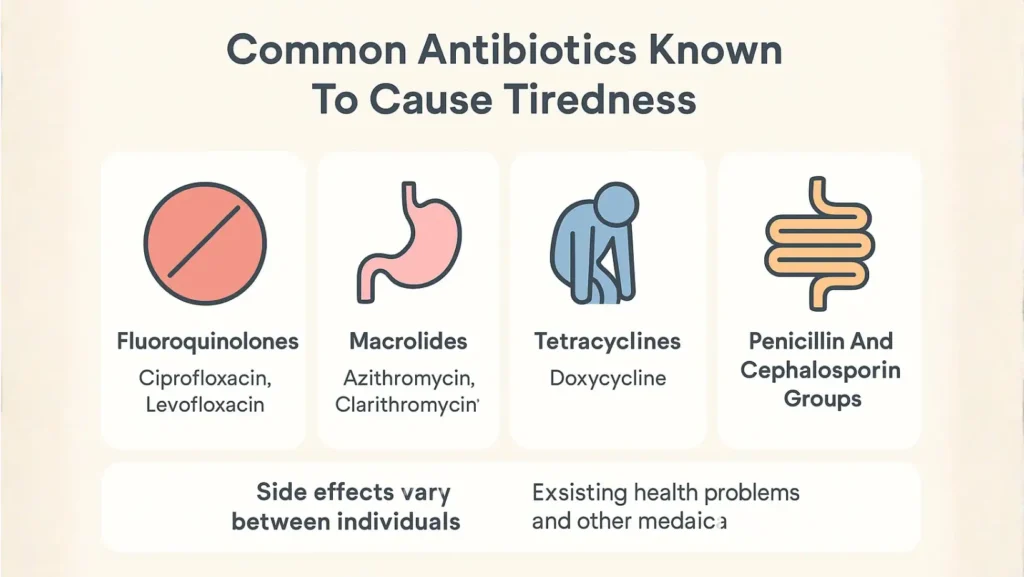
Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin)
These are powerful antibiotics. They sometimes damage nerves or tendons. They often cause dizziness or weakness. Many patients report fatigue or a sense of heaviness when using them.
Macrolides (e.g., Azithromycin, Clarithromycin)
Macrolides may irritate the stomach. They can alter how other drugs behave. You may feel weak or sleepy on them. Some people get mental fuzziness or lethargy.
Tetracyclines (e.g., Doxycycline)
Doxycycline is common. It can lead to nausea or sun sensitivity. If nausea causes you to eat less, you may lose energy. You may also feel tired as a side effect.
Penicillin And Cephalosporin Groups
These are widely used antibiotics. Usually well tolerated, but side effects like diarrhea, allergic reactions, or gut disturbance can cause fatigue. Some people feel do antibiotics make you tired and weak when using them.
Why Side Effects Vary Between Individuals
Side effects vary widely. Age, body weight, existing health problems, and other medications all play a role. For example, if you combine antibiotics with painkillers or antihistamines, your drowsiness may increase.
Difference Between Fatigue From Infection Vs. Medication
How Infection-Related Fatigue Works
During illness, your body directs energy to heal. You may have fever, aches, and poor sleep. All these consume energy. That fatigue tends to improve as infection goes away.
Clues That Fatigue Comes From The Antibiotic, Not The Illness
If your fever is gone but you still feel weak, the drug might be to blame. If fatigue appears right after you start medication, or worsens with each dose, suspect the antibiotic. If side effects start after beginning treatment, it could mean that taking antibiotics makes you tired.
Why Your Energy Might Drop Even After Recovery Begins
Even when infection fades, your gut may still be imbalanced. Nutrients may remain low. Mitochondria may need repair. So you may feel tired weeks after finishing antibiotics. That residual fatigue is common.
Other Side Effects That Can Make You Feel More Tired
Digestive Issues And Appetite Loss
Antibiotics often cause nausea, diarrhea, bloating, or stomach pain. These make you eat less. With less fuel, your body becomes weak and tired.
Mild Dehydration And Electrolyte Imbalance
Because of vomiting or diarrhea, you lose water and salts. Dehydration reduces blood flow and makes you sluggish. Low sodium or potassium (electrolytes) can worsen fatigue.
Sleep Disturbances Caused By Medication Timing
Some antibiotics may cause insomnia or daytime drowsiness. If taken late at night, they can interrupt your sleep cycle. Poor sleep makes your daytime energy slump.
Mental Fatigue Or Brain Fog
Brain fog means slow thinking, poor focus, and confusion. Some antibiotics cross into the brain and cause this. Mental tiredness feels heavier than normal sleepiness. It makes simple tasks harder.
How To Manage And Reduce Fatigue During Antibiotic Use
Stay Hydrated And Eat Energy-Rich Whole Foods
Drink water, herbal tea, broths. Eat lean protein, whole grains, and colorful veggies. Fruit and nuts help. These foods support your body and gut. That fights fatigue.
Add Probiotics To Support Gut Recovery
Use yogurt, kefir, sauerkraut, or probiotic supplements. Take probiotics a few hours apart from antibiotics. This may help reduce gut damage. It helps restore energy faster.
Get Enough Rest Without Total Inactivity
Rest when you feel tired. But try light movement too, short walks or stretching. Activity boosts circulation and mood. Balance rest and gentle movement.
Avoid Alcohol, Smoking, And Energy Drinks
Alcohol and smoking both hurt gut health and liver. They drain energy. Energy drinks may give a jolt, then crash your system. Avoid them while on antibiotics.
Check For Drug Or Supplement Interactions
Tell your doctor about all medicines, vitamins, or herbs you take. Some substances lessen the effectiveness of antibiotics or worsen side effects. Interactions may amplify fatigue. Always double-check.
Recovery After Antibiotic Treatment
How Long Fatigue Usually Lasts Post-Medication
For many people, fatigue declines in one or two weeks. But for some, tiredness lingers for days or weeks more. If fatigue lasts beyond four weeks, it’s wise to check with a healthcare provider.
Steps To Regain Strength And Energy Naturally
Return to good nutrition, hydration, and rest.
- Slowly increase physical activity.
- Try gentle exercise.
- Add vitamins if recommended.
- Let your body recharge.
Importance Of Rebuilding Gut Flora After A Course
- Help friendly bacteria grow again.
- Eat fiber and fermented foods.
- Use probiotics.
A healing gut restores digestion, drives nutrient absorption, and supports energy long term.
How To Prevent Tiredness In Future Antibiotic Courses
Talk To Your Doctor Before Starting A New Antibiotic
- Ask about side effects.
- Ask if gentler options exist.
- Mention your prior fatigue.
Your doctor may choose a drug that is less likely to make you weak.
Ask About Gentler Alternatives Or Probiotic Support
You can request antibiotics that spare good gut bacteria. Ask whether taking probiotics or diet changes from day one will help. That may reduce the effect.
Take Medication Exactly As Prescribed
Do not skip doses or stop early. Finishing the full course protects against returning infection. That relapse would sap more energy. Following instructions also reduces side effects.
Supportive Diets That Protect Energy Levels
Plan your meals around protein, fruits, vegetables, and whole grains.
- Eat small but frequent meals if your appetite drops.
- Drink plenty of fluids.
- Avoid junk food that drains you more.
FAQs
Why do antibiotics make some people feel tired?
Antibiotics can disrupt gut bacteria, cause immune reactions, and affect mitochondria, all leading to fatigue. That is why antibiotics make you tired.
Are certain antibiotics more likely to cause fatigue?
Yes. Antibiotics like fluoroquinolones or macrolides often cause greater fatigue. But any antibiotic may trigger tiredness, depending on your body and dose.
How long does antibiotic tiredness usually last?
It often lasts one to two weeks after finishing the drug. But in some cases, fatigue may persist longer. If it goes beyond four weeks, ask your doctor.
Can probiotics help reduce antibiotic-related fatigue?
Probiotics restore good gut bacteria. That helps digestion and nutrient absorption. Better gut health often reduces fatigue. So yes, probiotics may reduce antibiotic fatigue.
Should I stop my antibiotics if I feel weak?
No. Do not stop antibiotics on your own. Stopping may let the infection return and worsen fatigue. Instead, tell your doctor immediately about severe weakness.
Can antibiotics affect my sleep quality?
Yes. Some antibiotics may cause insomnia or daytime sleepiness. They may alter your sleep cycle. Poor sleep deepens the feeling of tiredness.
Is tiredness a sign that the antibiotic is working?
Tiredness is not a reliable sign of success. It is more likely a side effect or part of your immune response, not an indicator that the drug is effective.
What foods can help restore energy during treatment?
Eat lean protein, whole grains, fruits, vegetables, and fermented foods. Drink water. Avoid sugar and processed snacks. Balanced meals fuel recovery.
When should I talk to a doctor about fatigue?
Speak to a doctor if fatigue is extreme, sudden, or disrupts daily life. Also if it lasts more than four weeks, or you have chest pain, fainting, or shortness of breath.
How do I recover faster after finishing antibiotics?
Support gut health with probiotics and fiber. Eat nutritious foods. Sleep well. Increase activity slowly. If fatigue lasts long time, get a medical checkup.














Leave a Comment