Living with diverticulitis can be tough, but we have a nutrition guide to help. We know how hard it is to manage diverticulitis with diet. Our guide offers expert tips to prevent flare-ups and keep your digestive system healthy.
Diverticulitis is common, affecting millions in the U.S. By age 60, half of adults have diverticula in their colon. Our diet plan helps you choose foods that reduce symptoms and improve health.
Nutrition is key in managing diverticulitis. Most Americans eat only 10-15 grams of fiber a day. Our guide shows how changing your diet can lower the chance of flare-ups and boost digestive health.
If you’re facing your first diverticulitis episode or dealing with it long-term, this guide is for you. We’ll share tips on making a diet that’s good for your digestive system and overall health.
Understanding Diverticulitis and Its Dietary Impact
Diverticular disease is a common digestive problem. It affects millions globally. It’s especially common in people over 60, so knowing about it is key.
What is Diverticulitis?
Diverticulitis happens when small pouches in the colon wall get inflamed or infected. These pouches form when the intestinal wall weakens. Only a small percentage of people with diverticulosis get diverticulitis, which is good news.
How Diet Affects Diverticular Disease
What you eat can help manage diverticulitis. Eating less fiber and more red meat might raise your risk. The right diet can help reduce inflammation and support your digestive system
- Aim for 28 grams of dietary fiber daily
- Choose foods with at least 3 grams of fiber per serving
- Gradually increase fiber intake to allow body adjustment
Signs and Symptoms
Knowing the symptoms of diverticulitis is important. Look out for stomach pain, fever, and changes in bowel movements. The pain can be mild or severe, depending on the inflammation.
Doctors suggest drinking plenty of water and eating foods high in fiber. Most Americans don’t get enough fiber, making diet a big part of managing diverticular disease.
Clear Liquid Diet During Flare-Ups

Managing acute diverticulitis needs a smart plan for what you eat. When you have a flare-up, doctors often suggest a clear liquid diet. This lets your digestive system rest and heal.
This diet is made of drinks that are easy to digest. They don’t put a lot of stress on your intestines. It helps your body heal during a diverticulitis episode.
- Water
- Clear broths
- Pulp-free fruit juices
- Gelatin
- Herbal tea
- Plain coffee
- Ice chips
People with diverticulitis usually eat only clear liquids for one to three days. The main goal is to let your intestines heal. It also keeps you hydrated and gives some nutrition.
Our medical team says it’s key to slowly move from clear liquids to a low-fiber diet. This helps your digestive system not get too stressed. It also helps your healing keep going.
Always talk to a doctor to make a diet plan that fits your needs. This plan should match your diverticulitis symptoms and health.
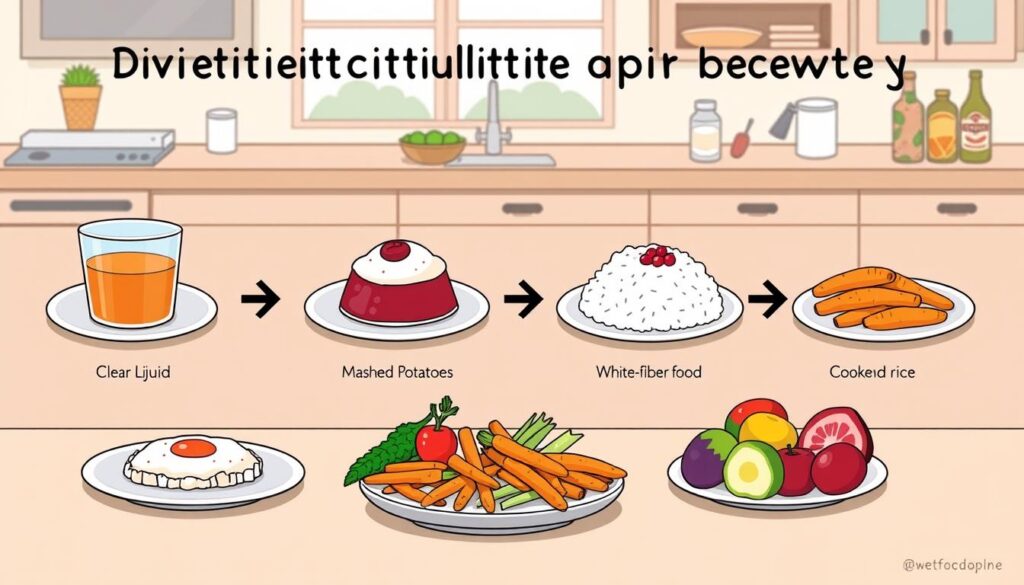
Best Diet for Managing Diverticulitis: Stage-by-Stage Approach
Managing diverticulitis needs a careful diet plan. Our guide will help you understand each diet stage easily.
Diverticulitis affects 5-25% of those with diverticulosis. A special diet is key to managing it well. We’ll cover each diet phase.
Acute Phase Diet
In the acute phase, you aim to reduce digestive stress. Doctors often suggest a clear liquid diet. This lets your digestive system rest and heal.
- Clear liquids like water, broth, and pulp-free juices
- Herbal tea
- Sports drinks
- Gelatin
Recovery Phase Diet
When you move past the acute phase, your diet changes. Start adding low-fiber foods that are easy on your stomach.
- Scrambled eggs
- White toast
- Skinless fruits
- Smooth, creamy foods
- Lean proteins
Maintenance Phase Diet
The maintenance diet aims for long-term digestive health. Eating 30-40 grams of fiber daily can lower disease risk by 41-58%.
- High-fiber vegetables
- Whole grains
- Legumes
- Fruits with edible skins
Always talk to your doctor to tailor these diets to your health and symptoms.
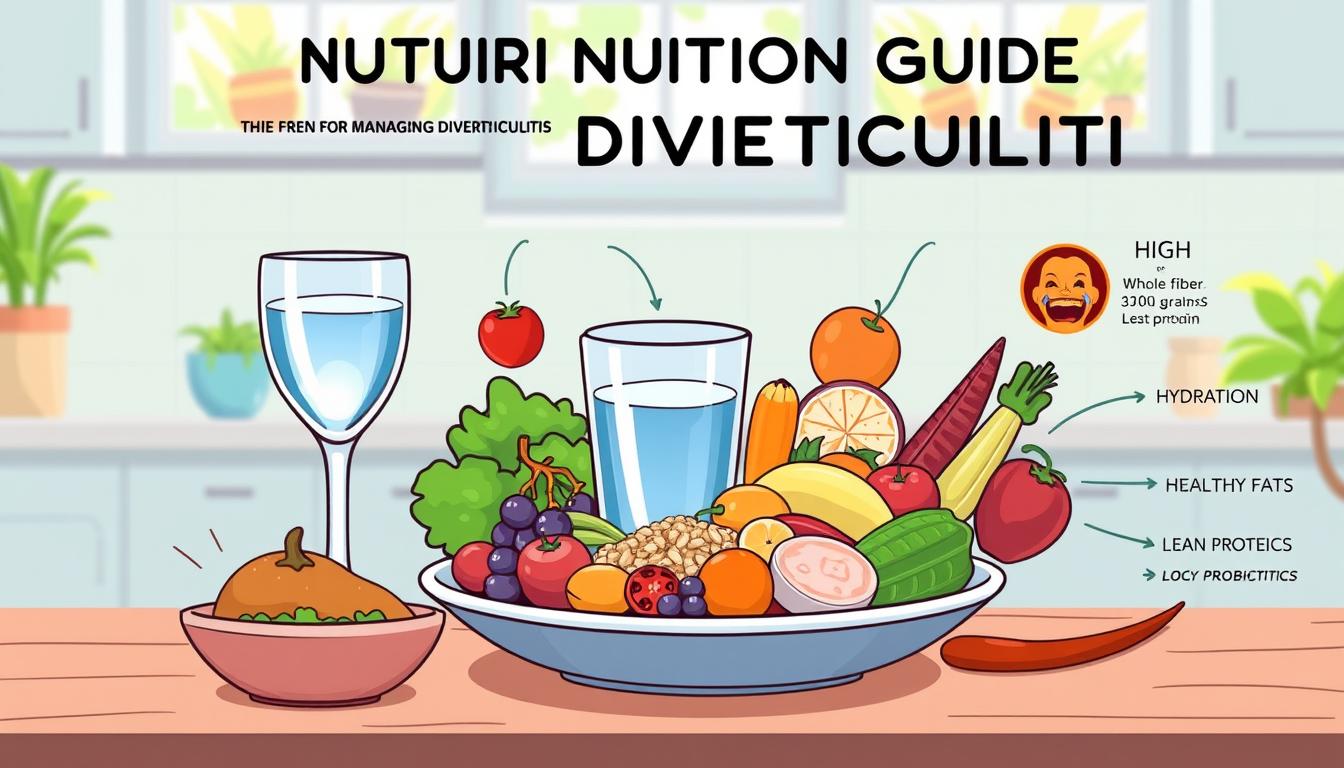
Essential High-Fiber Foods for Prevention
Preventing diverticulitis starts with a fiber-rich diet. Our digestive health needs foods high in fiber. These foods help our colon work well and lower inflammation risks.
To prevent diverticulitis, add high-fiber foods to your meals. Studies show that enough fiber can lower the risk of this digestive problem.
- Whole Grains: Quinoa, brown rice, and whole wheat bread
- Legumes: Black beans, lentils, and chickpeas
- Vegetables: Broccoli, spinach, and kale
- Fruits: Apples, pears, and berries with edible skins
We suggest eating 25-30 grams of fiber each day. This helps keep bowel movements regular and lowers colon pressure. Slowly adding more fiber is important to avoid stomach upset.
Soluble and insoluble fibers are important for preventing diverticulitis. Soluble fibers, like oats and beans, help good gut bacteria. Insoluble fibers, from wheat bran and veggies, make stools bulky and help digestion.
Don’t forget to drink lots of water when eating more fiber. Water helps these foods prevent diverticulitis flare-ups.
Foods to Avoid During Flare-Ups
Managing diverticulitis means watching what you eat closely. Knowing which foods can trigger flare-ups is key. This guide will help you understand which foods to avoid and how to safely add them back in.
Identifying Common Trigger Foods
Some foods can make diverticulitis worse. It’s best to avoid these:
- Red and processed meats
- Refined grains
- Full-fat dairy products
- Fried foods
- Raw fruits and vegetables
- Foods with small seeds or nuts
Temporary Food Restrictions
When you have diverticulitis, eat foods that are easy to digest. Start with a clear liquid diet. Then, slowly add soft foods back into your diet.
- Eggs
- Lean proteins like chicken and fish
- White bread
- Rice and pasta
- Canned or cooked fruits
- Low-fiber cereals
Safely Reintroducing Foods
Adding foods back into your diet needs to be done carefully. Work with your doctor to make a plan. Start with foods that are low in fiber and slowly add more as you feel better. Pay attention to how your body reacts to different foods.
A 2017 study showed that avoiding certain foods and eating more fruits, veggies, and whole grains can help. It can also make symptoms better.
Transitioning Back to Regular Diet
Going back to a normal diet after a diverticulitis flare-up takes time and planning. Our plan is to help your digestive system heal slowly. This way, it can get stronger again.
When you’re on the diverticulitis recovery diet, we suggest a step-by-step plan. This plan focuses on your digestive health. It involves slowly adding foods back into your diet to avoid problems.
- Start with low-fiber foods that are gentle on the digestive system
- Gradually increase fiber intake over several weeks
- Monitor your body’s response to new foods
- Stay hydrated throughout the transition
The first step in going back to a normal diet is to eat foods that are easy to digest. These include:
- White bread and pasta
- Well-cooked vegetables
- Lean proteins like chicken and fish
- Low-fat dairy products
About 10-20% of people with diverticular conditions need to watch what they eat. Our goal is to help you safely go back to a high-fiber diet. This diet supports your digestive health and helps prevent future problems.
Keep in mind that everyone’s body is different. Work with your healthcare provider to make a plan that fits your needs. This will help you recover smoothly.
Daily Fiber Requirements and Guidelines
Knowing how much fiber you need is key for good digestion. Fiber helps your bowels work right and keeps many stomach problems away. Let’s look at how to meet your dietary fiber needs.
Recommended Fiber Intake by Age and Gender
Fiber needs change with age, gender, and how many calories you eat. Here’s what you should aim for:
- Adult women under 50: 25 grams per day
- Adult women over 50: 22 grams per day
- Adult men under 50: 31 grams per day
- Adult men over 50: 28 grams per day
Tips for Increasing Dietary Fiber
It’s easy to get more fiber. Here are some tips:
- Choose whole grains over refined ones
- Add beans to your meals
- Snack on fruits and vegetables
- Include nuts and seeds in your diet
- Slowly add more fiber to avoid stomach upset
Great fiber foods include raspberries (8 grams per cup), green peas (8.8 grams per cup), and lentils (7.8 grams per half cup). Drink lots of water when you eat more fiber to help with digestion.
Hydration and Its Role in Prevention

Drinking water is key to stopping diverticular disease and keeping your gut healthy. Our bodies need water to digest food well and avoid diverticulitis.
Learning how water helps prevent diverticulitis is important. Drinking enough water helps your body digest food better. It also lowers the chance of getting diverticulitis.
- Aim to consume water based on body weight
- Drink approximately half your body weight in ounces daily
- Support fiber effectiveness through consistent hydration
- Promote regular bowel movements
But water isn’t the only thing that helps. Soft drinks like herbal teas and clear broths are good too. They keep your gut healthy and give you important nutrients.
Studies show that drinking water often can lower the risk of diverticulitis. People who drink enough water have fewer problems with inflammation and digestion.
- Supports intestinal tract lubrication
- Helps prevent constipation
- Reduces strain during bowel movements
- Minimizes potential diverticular complications
It’s smart to talk to a doctor about how much water you should drink. They can help you make a plan that fits your health and what you eat.
Meal Planning Strategies for Diverticulitis
Planning meals for diverticulitis needs careful thought and a smart plan. Over 2.5 million Americans have this condition. It’s key to know how to eat well to manage symptoms and stop flare-ups.
Good meal planning for diverticulitis means making meals that are good for your gut and don’t cause inflammation. We focus on portion control and picking foods wisely. This helps people with diverticulitis manage their condition well.
Sample Meal Plan Strategies
- Create 5-6 small meals daily to ease digestion
- Incorporate soluble and insoluble fiber sources gradually
- Include lean proteins and healthy fats
- Choose easily digestible foods during recovery
Portion Control Guidelines
Using portion control is key for a good diet with diverticulitis. We suggest the plate method:
- Half plate: Non-starchy vegetables
- Quarter plate: Lean proteins
- Quarter plate: Whole grains
Adjust your meal plans based on how you feel and your symptoms. Talking to a healthcare professional can help make a diet plan that works for you.
About 75% of diverticulitis cases are mild. They can be managed with lifestyle changes. By planning meals carefully and controlling portions, you can improve your gut health. This can also lower the chance of future flare-ups.
The Truth About Nuts, Seeds, and Popcorn

For years, people with diverticular disease were told to avoid nuts and seeds. But recent research has changed this advice. Nuts and seeds are not as bad as we thought. They can actually help with digestive health.
A study in The Journal of the American Medical found no bad link. It showed nuts, seeds, and diverticular disease are not connected.
- Nuts are rich in fiber and can support digestive health
- Seeds provide essential nutrients that may help prevent inflammation
- Popcorn is now considered a safe food for most individuals with diverticulitis
When you have acute diverticulitis, you should avoid these foods for a while. But once you feel better, you can start eating them again. It’s important to talk to your doctor about how much you can eat.
It’s all about eating in moderation and listening to your body. While nuts and seeds have a tricky relationship with diverticular disease, doctors now say they can be part of a healthy diet. Just eat them carefully.
Supplements and Additional Dietary Considerations
Managing diverticulitis is more than just diet. Supplements are key for digestive health and symptom management. Our guide covers the best diverticulitis supplements and what patients should know.
Beneficial Supplements for Diverticular Disease
Probiotics for diverticular disease are getting more attention. They help restore gut health and may lower inflammation. Important supplements include:
- Probiotic strains for digestive health
- Fiber supplements for regular bowel movements
- Magnesium for strong intestinal muscles
- Vitamin D to reduce inflammation
Understanding Medication and Diet Interactions
Choosing supplements needs careful thought about interactions. Always talk to a healthcare provider before starting new supplements. Key points to remember are:
- Antibiotics for diverticulitis might interact with some supplements
- When you take supplements can affect medication
- Some supplements might block how medications are absorbed
A 2019 study found probiotics with antibiotics can lessen abdominal pain in diverticulitis. Research shows the right supplements can help digestive health.
Work with your healthcare provider to create a supplement plan. It should meet your diverticulitis management needs.
Conclusion
Managing diverticulitis through diet is a long-term commitment to your gut health. Diverticular disease affects up to 65% of people over 85. So, it’s key to understand how to support your gut as you get older.
Studies show that a good diet can lower your risk of diverticulitis. Eating foods high in fiber, like whole grains, fruits, and veggies, can cut your risk by up to 58%. The goal is to make healthy eating a part of your life for good.
Being healthy is more than just what you eat. Exercise, managing stress, and drinking enough water are also important. Our bodies do best when we take care of them in a holistic way.
Every person’s battle with diverticulitis is different. Working with your doctor, staying up-to-date on nutrition research, and listening to your body are key. This will help you find the best way to take care of your digestive health.
FAQ
What is diverticulitis?
Diverticulitis is when small pouches in the colon wall get inflamed or infected. It can cause stomach pain, fever, and changes in bowel movements. Eating the right foods is key to managing and preventing it.
What diet should I follow during an acute diverticulitis flare-up?
When you’re having a flare-up, doctors often suggest a clear liquid diet. This means drinking broths, clear juices, water, and ice pops. As you start to feel better, you can slowly add in low-fiber foods and then more fiber-rich ones.
How much fiber should I consume daily?
The amount of fiber you need depends on your age and gender. Women under 50 should get at least 25g of fiber a day. Those over 50 need 22g. Men under 50 should aim for 31g, and over 50, 28g. Increase your fiber intake slowly and drink plenty of water to avoid stomach discomfort.
Are nuts and seeds safe to eat if I have diverticulitis?
Recent studies show that nuts, seeds, and popcorn don’t raise the risk of diverticulitis. But during flare-ups, it’s best to avoid them and add them back in slowly once your symptoms get better.
What foods should I avoid during a diverticulitis flare-up?
During flare-ups, stay away from high-fiber foods, raw fruits and veggies, and foods with small seeds or nuts. Also, limit dairy and fatty foods. Start with low-fiber foods as your symptoms improve.
How important is hydration for managing diverticulitis?
Drinking enough water is crucial for preventing diverticulitis and keeping your digestive system healthy. Try to drink half your body weight in ounces of water each day. Drinking enough water helps fiber work better, softens your stools, and keeps your bowel movements regular.
Can supplements help manage diverticulitis?
Some supplements, like probiotics, can support your gut health. Fiber supplements can also help meet your daily fiber needs. But always talk to a healthcare provider before starting any supplements to avoid any bad interactions.
What does a typical meal plan for diverticulitis look like?
A good meal plan balances fiber, portion sizes, and variety. Eat 5-6 small meals a day, using the plate method (half veggies, quarter protein, quarter grains). Adjust the plan based on how you feel and your symptoms.
How do I transition back to a regular diet after a flare-up?
Begin with low-fiber foods like white bread, pasta, and well-cooked veggies. Slowly add in more fiber-rich foods over weeks. Watch your symptoms and adjust as needed. The goal is to get back to a high-fiber diet to prevent future flare-ups.












Leave a Comment