Obesity hypoventilation syndrome is a health condition where extra body weight makes it hard to breathe normally. It causes a rise in carbon dioxide and a drop in oxygen, leading to serious health risks if not managed properly. Doctors also call it Obesity hypoventilation syndrome (OHS) (Pickwickian syndrome). This guide explains the symptoms, causes, diagnosis, treatment, prevention, and long-term outlook of OHS in simple language.
Table of Contents
ToggleOverview
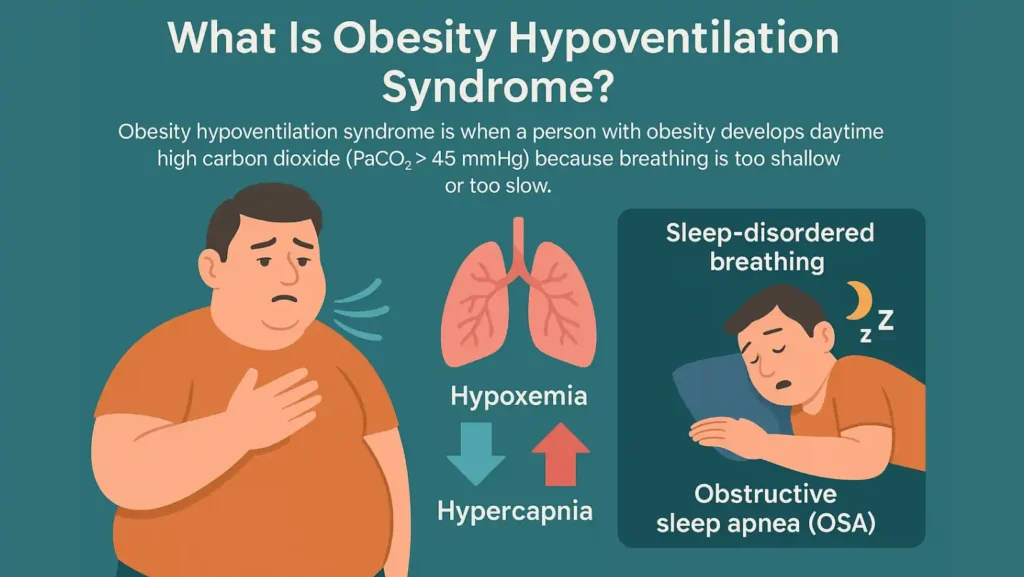
What Is Obesity Hypoventilation Syndrome?

Obesity hypoventilation syndrome is when a person with obesity develops daytime high carbon dioxide (PaCO₂ > 45 mmHg) because breathing is too shallow or too slow. Unlike regular obesity, this condition involves a specific breathing problem.
Obesity hypoventilation syndrome is a breathing disorder in obesity where the lungs cannot move enough air. As a result, oxygen falls too low (Hypoxemia) and carbon dioxide rises too high (Hypercapnia).
This condition is often linked with Sleep-disordered breathing such as obstructive sleep apnea (OSA). Most people with OHS also have OSA, but OHS is more serious because it affects breathing even during the day.
Who Does OHS (Obesity Hypoventilation Syndrome) Affect?
OHS obesity affects adults with high BMI (Body mass index), usually above 30. The risk rises with severe obesity. Men are slightly more affected, but women are not spared. It can affect any age group, though middle-aged and older adults are more commonly diagnosed.
People with OHS often also have obstructive sleep apnea (OSA), high blood pressure, type 2 diabetes, and metabolic syndrome. These overlapping conditions increase the burden on the body.
How Common Is Obesity Hypoventilation Syndrome?
The true number of people with OHS obesity hypoventilation syndrome is underestimated. In the general population, fewer than 1 in 100 adults are affected. But among those with severe obesity or with sleep apnea, the rates climb as high as 10–30 percent. Many cases remain undiagnosed because daytime symptoms are mistaken for simple tiredness or depression.
Symptoms and Causes
What Are The Symptoms Of Obesity Hypoventilation Syndrome?
Obesity hypoventilation syndrome symptoms develop slowly and can be confused with other health issues. The most common signs include:
- Shortness of breath with little activity
- Fatigue, lack of energy, sluggishness
- Morning headaches from poor overnight breathing
- Dizziness and Depression
- Loud snoring, choking, gasping, pauses in breathing during sleep
- Daytime sleepiness and trouble concentrating
Low oxygen and high carbon dioxide explain many of these symptoms. Repeated drops in oxygen at night disturb sleep and cause strain on the heart and blood vessels.
What Causes Obesity Hypoventilation Syndrome?
The causes of obesity hypoventilation syndrome are linked to both body structure and brain signals.
- Mechanical load on the chest: Extra fat around the chest and belly makes it harder for the lungs to expand. This limits air movement.
- Weakened breathing drive: Hormonal imbalances such as leptin resistance reduce the brain’s drive to breathe deeply.
- Sleep-disordered breathing: Most patients have obstructive sleep apnea (OSA), which worsens breathing problems at night.
Together, these factors create an oxygen and carbon dioxide imbalance, leading to chronic hypoventilation and long-term risk of respiratory failure in obesity.
Diagnosis and Tests
How Is Obesity Hypoventilation Syndrome Diagnosed?
Doctors rely on clinical signs and tests. The gold standard is Arterial blood gas testing that shows daytime carbon dioxide (PaCO₂) above 45 mmHg.
Other important diagnostic tools include:
- Pulse oximeter to measure oxygen levels
- Pulmonary function tests to check lung capacity
- Chest X-ray to rule out other conditions
- Sleep study (Polysomnography) to assess sleep apnea
- Blood tests for thyroid and hormone levels
A diagnosis of OHS requires obesity, daytime hypercapnia, and the exclusion of other causes such as neuromuscular disease or chronic lung disease.
Management and Treatment
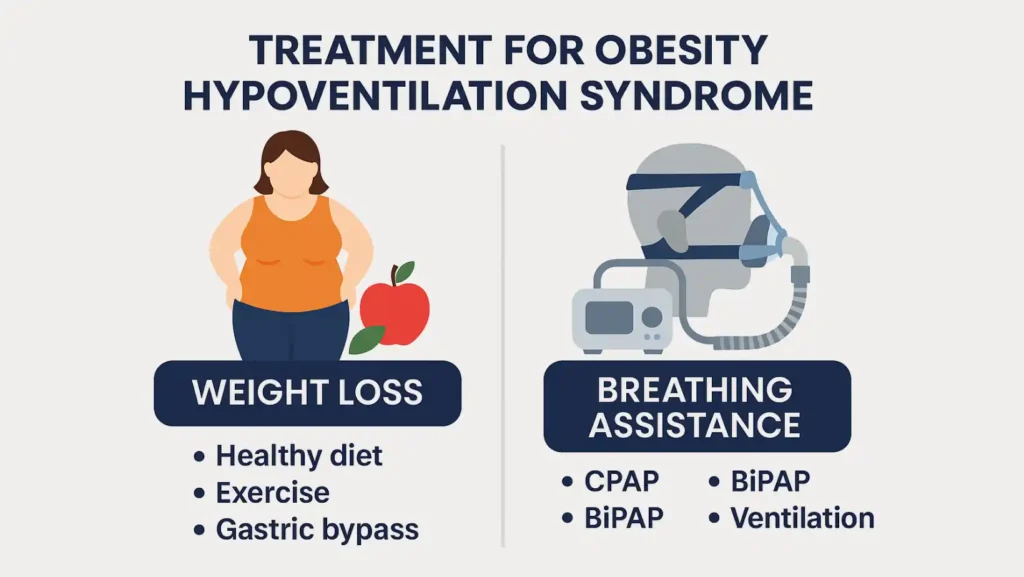
What Is The Treatment For Obesity Hypoventilation Syndrome?

Treatment for obesity hypoventilation syndrome focuses on improving breathing and reducing weight. Since OHS can cause life-threatening complications, treatment must be started quickly once diagnosed.
The two main approaches are weight loss and breathing assistance.
Weight Loss as a Treatment for OHS
Weight loss reduces the physical strain on the chest and lungs. Even a modest 10% weight reduction can improve oxygen levels.
Methods include:
- Healthy diet plans such as the Mediterranean diet
- Increased physical activity under medical supervision
- Behavioral therapy for long-term weight control
- Gastric bypass surgery for severe obesity when other methods fail
Weight loss not only improves breathing but also lowers blood pressure, reduces diabetes risk, and prevents cardiopulmonary complications.
Breathing Assistance (CPAP, BiPAP, Or Ventilatory Support)
The second key treatment for obesity hypoventilation syndrome is breathing support.
- CPAP (Continuous Positive Airway Pressure): Keeps the airway open at night, helping oxygen levels stay stable.
- BiPAP (Bilevel Positive Airway Pressure): Provides two pressure levels, making it easier for patients with high carbon dioxide to exhale.
- Non-invasive ventilation (NIV): Advanced settings that control both oxygen and carbon dioxide balance.
- Tracheostomy: Rarely needed, but can be used in severe cases where other options fail.
These treatments prevent respiratory failure in obesity and improve sleep quality. Doctors also carefully monitor oxygen therapy because too much oxygen can worsen carbon dioxide retention.
Outlook / Prognosis
What Is The Life Expectancy Of Someone With Obesity Hypoventilation Syndrome?
Without treatment, OHS greatly shortens life expectancy due to pulmonary hypertension, right-sided heart failure, and other heart and blood vessel issues. With proper care, survival improves dramatically. Patients using CPAP or BiPAP regularly have a much better outlook. Weight loss further extends life expectancy by reducing the strain on the lungs and heart.
What Are The Possible Complications Of OHS?
ohs obesity hypoventilation syndrome can lead to serious complications if left untreated:
- Pulmonary hypertension
- High blood pressure (hypertension)
- Right-sided heart failure
- Mortality (shortened life expectancy)
- Recurrent hospital admissions for breathing crises
These complications highlight why early diagnosis and treatment are crucial.
Prevention
How Can I Reduce My Risk Of Obesity Hypoventilation Syndrome?
Prevention focuses on maintaining a healthy weight and good sleep habits. Steps include:
- Weight loss through diet and exercise
- Following sleep hygiene like regular bedtimes and avoiding alcohol before sleep
- Using CPAP or BiPAP as prescribed if diagnosed with sleep apnea
- Avoiding smoking and substances that slow breathing
- Regular doctor visits to track BMI and breathing tests
Prevention (healthy weight, CPAP, BiPAP adherence) lowers the chances of developing OHS and protects against life-threatening complications.
The Bottom Line
Obesity hypoventilation syndrome is more than just snoring or being overweight. It is a dangerous breathing disorder linked to high carbon dioxide, low oxygen, and serious heart risks. The good news is that it is treatable. With proper diagnosis, treatment for obesity hypoventilation syndrome like CPAP, BiPAP, and structured weight loss, people can breathe better, sleep better, and live longer. Early detection and consistent care make all the difference.
FAQs
How is obesity hypoventilation syndrome treated?
It is treated with weight loss programs, CPAP or BiPAP therapy, and sometimes gastric bypass surgery. Oxygen may be added under careful supervision.
What are the criteria for OHS syndrome?
Obesity, daytime carbon dioxide above 45 mmHg, and exclusion of other conditions are required. Sleep studies and blood tests confirm the diagnosis.
Can OHS be cured?
With major weight loss and proper therapy, many patients see symptoms reverse. Others may need long-term CPAP or BiPAP to control the condition.
How to differentiate between OSA and OHS?
OSA affects breathing during sleep only. OHS causes daytime carbon dioxide buildup. Blood gas tests help doctors separate the two.
How do I know if I have OHS?
If you are obese, have loud snoring, morning headaches, or constant tiredness, see a doctor. Testing is needed for confirmation.
What are the symptoms of OHS?
Symptoms include shortness of breath, fatigue, morning headaches, dizziness, depression, and loud snoring with pauses in breathing at night.
Is OHS a restrictive lung disease?
Yes, OHS causes a restrictive pattern because chest wall expansion is limited by body fat. Pulmonary function tests confirm this pattern.

This article is medically reviewed by Dr. Chandril Chugh, Board-Certified Neurologist, providing expert insights and reliable health information.
Dr. Chandril Chugh is a U.S.-trained neurologist with over a decade of experience. Known for his compassionate care, he specializes in treating neurological conditions such as migraines, epilepsy, and Parkinson’s disease. Dr. Chugh is highly regarded for his patient-centered approach and dedication to providing personalized care.