Hormonal acne is a type of acne that is different from the usual teenage breakouts. It is deeply connected to your hormones, which means no single cream can fix it overnight. To truly treat hormonal acne, you must understand why it happens, how your body reacts, and what treatments (both medical and natural) can actually help.
Table of Contents
ToggleWhat Is Hormonal Acne?
Hormonal acne happens when your hormone levels, mainly androgens (male hormones found in both men and women), fluctuate and cause your skin’s oil glands to produce excess sebum (natural oil). When this oil mixes with dead skin cells, your pores clog, bacteria grow, and acne forms.
How Hormones Trigger Breakouts and Excess Oil Production
Your skin’s oil glands are sensitive to hormones, especially androgens. When these hormones rise (during puberty, menstrual cycles, pregnancy, or stress), your skin makes more oil. This extra oil traps bacteria and dirt, forming pimples, blackheads, or deep cysts. That’s why treating hormonal acne often starts with controlling these hormone fluctuations.
Common Areas Affected by Hormonal Acne
Hormonal acne typically affects the lower part of your face, especially:
- Chin
- Jawline
- Neck
- Around the mouth
These areas have more oil glands that respond to hormone changes. The acne in these spots is usually painful, cystic, and harder to pop.
Key Differences Between Hormonal and Bacterial Acne
Hormonal acne forms deeper, painful cysts that don’t come to a whitehead. Bacterial acne, on the other hand, usually appears as small pimples or whiteheads. Hormonal acne also tends to come back in cycles, especially around menstruation or periods of stress.
How Common Is Hormonal Acne in Adults?
It’s extremely common. Around 50% of women in their 20s and 30s experience adult acne caused by hormones. Men can also get it, though less often. Many people think acne ends after their teenage years, but adult hormonal acne proves otherwise.
What Causes Hormonal Acne?
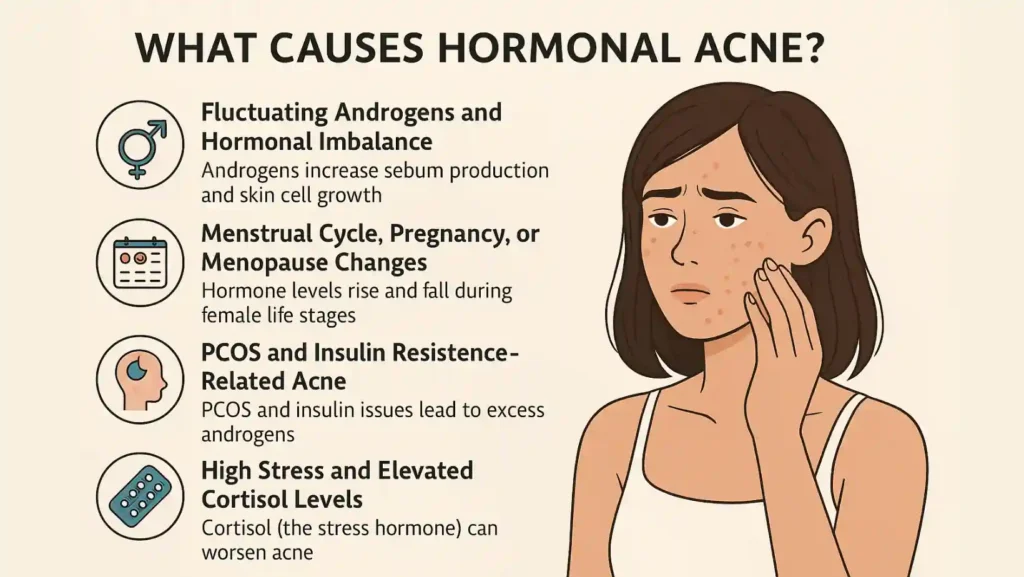
Fluctuating Androgens and Hormonal Imbalance
Androgens increase sebum production and skin cell growth. Too much oil clogs pores, leading to inflammation and acne. This hormonal imbalance can happen naturally or due to medical conditions.
Menstrual Cycle, Pregnancy, or Menopause Changes
Your hormone levels rise and fall during your menstrual cycle, causing monthly breakouts. Pregnancy also alters hormone levels, which can either improve or worsen acne. During menopause, estrogen drops, leading to relative increases in androgens, which can trigger acne again.
PCOS and Insulin Resistance–Related Acne
Polycystic Ovary Syndrome (PCOS) is one of the most common causes of hormonal acne in women. PCOS causes excess androgens, irregular periods, and insulin resistance (a condition where your body struggles to use sugar). These hormone changes often cause deep, painful acne on the face and body.
High Stress and Elevated Cortisol Levels
When you’re stressed, your body produces cortisol, the stress hormone. Cortisol can increase oil production and worsen acne. That’s why treating hormonal acne also includes managing stress.
Certain Medications and Contraceptive Changes
Some drugs, including steroids and certain birth controls, can trigger acne. Even switching contraceptives may cause hormone shifts that lead to new breakouts. Always consult a doctor before making medication changes.
Signs You May Have Hormonal Acne
- Painful, deep cysts that last for weeks
- Breakouts that appear around your period or during stressful times
- Acne that doesn’t respond to normal over-the-counter treatments
- Oily skin, especially around the chin, jawline, or lower cheeks
These symptoms mean your acne is more than just clogged pores; it’s hormone-driven.
Best Treatments for Hormonal Acne (FS Optimized)
If you want to treat hormonal acne , you need both medical and lifestyle strategies. Here are the most effective treatments doctors often recommend.
Topical Retinoids (Adapalene, Tretinoin)
Retinoids help clear pores by speeding up skin renewal. They prevent new breakouts and improve skin texture. Start with a small amount at night, as retinoids can cause dryness.
Oral Contraceptives
Certain birth control pills regulate estrogen and progesterone levels, which help reduce oil production. Pills like Yaz or Ortho Tri-Cyclen are often prescribed for acne-prone women.
Anti-Androgen Medications Like Spironolactone
Spironolactone blocks androgen hormones and lowers sebum levels. It’s very effective for adult women with stubborn acne that doesn’t improve with creams or antibiotics.
Short-Term Antibiotics
Antibiotics can quickly reduce inflammation and bacterial growth. They’re not a long-term fix, but can be used for severe cases along with other treatments.
Hormone-Balancing Therapies
In cases of PCOS or menopause, doctors might use hormone therapy to balance your levels. Always use these treatments under medical supervision.
How to Treat Hormonal Acne Naturally at Home? Natural & At-Home Remedies

To treat hormonal acne naturally at home , you can support your skin with gentle, evidence-backed methods. These work best for mild to moderate acne or as add-ons to medical treatment.
Tea Tree Oil and Sulfate-Free Cleansers
Tea tree oil has antibacterial properties. Mix a few drops with a carrier oil or use skincare products containing it. Avoid harsh soaps; they strip skin and trigger more oil.
Green Tea and Antioxidants
Green tea is rich in antioxidants that calm inflammation. You can drink it daily or use skincare products with green tea extract. It helps reduce redness and oil buildup.
Limiting Dairy and Sugar
Dairy, especially milk, can raise insulin and androgen levels. Sugary foods cause insulin spikes that worsen acne. Reduce both for clearer skin.
Omega-3s and Zinc
Omega-3 fatty acids (found in fish or flaxseed) and zinc supplements help reduce inflammation and regulate oil production. These support the body from within.
Stress Management and Sleep
Cortisol from stress increases oil production. Deep breathing, yoga, or simply sleeping 7-8 hours a night can balance hormones. This helps cure hormonal acne naturally over time.
How Your Diet Affects Hormonal Acne
High-Glycemic Foods and Insulin Spikes
White bread, soda, and sugary snacks increase insulin, leading to more oil and acne. Switch to low-glycemic foods like oats, lentils, and green vegetables.
Dairy’s Link with Hormone-Sensitive Acne
Dairy contains hormones that may interfere with your body’s own balance. Reducing dairy intake can help you see clearer skin within weeks.
Benefits of Whole, Plant-Rich Meals
Fruits, vegetables, and whole grains help detox your body naturally. Their antioxidants protect skin cells and improve healing.
Importance of Hydration
Water flushes out toxins and supports skin repair. Drink at least 2 liters of water daily to help get rid of hormonal acne faster.
Skincare Routine for Hormonal Acne
A consistent skincare routine is key to treating hormonal acne successfully.
Step 1: Cleanse
Use a gentle, non-stripping cleanser with salicylic acid or glycolic acid twice a day. It removes dirt, oil, and dead skin without drying your skin.
Step 2: Treat
Apply topical treatments like retinoids or niacinamide-based serums. These ingredients reduce oil and inflammation while keeping skin smooth.
Step 3: Moisturize
Even oily skin needs hydration. Use non-comedogenic (doesn’t clog pores) moisturizers to maintain a balanced barrier.
Step 4: Protect
Always wear broad-spectrum sunscreen. UV exposure can worsen scars and pigmentation after acne heals.
When to See a Dermatologist
You should see a dermatologist if:
- Acne lasts more than 3 months despite home care
- You have painful cysts that cause scarring
- Breakouts get worse with each menstrual cycle
- You have signs of PCOS, like irregular periods or facial hair
A doctor can identify hormone triggers and offer targeted medication or therapy.
Advanced Medical Options for Severe Hormonal Acne
If your acne doesn’t respond to regular treatments, advanced options are available:
- Laser and Light Therapy: Targets oil glands and kills acne bacteria.
- Chemical Peels and Microdermabrasion: Exfoliate and fade acne scars.
- Prescription Hormonal Therapy: Balances hormones in PCOS or menopausal acne.
These should always be done under expert supervision.
Long-Term Prevention & Skin Maintenance
Consistency matters more than intensity. Here’s how to keep hormonal acne away:
- Stick to a simple, gentle skincare routine.
- Manage stress with mindfulness or light exercise.
- Eat balanced meals and stay active.
- Avoid touching or picking pimples.
- Visit your dermatologist regularly to track progress.
Prevention means balancing your hormones and caring for your skin daily, not just treating flare-ups.
Frequently Asked Questions (FAQs)
What Causes Hormonal Acne Flare-Ups in Adults?
Hormonal acne flare-ups happen when hormones like androgens rise during stress, menstruation, or health conditions such as PCOS, increasing oil production and clogging pores.
Can Hormonal Acne Be Permanently Cured?
While there’s no permanent cure, consistent skincare, diet control, and medication can help cure hormonal acne naturally or medically for long-lasting results.
Is Hormonal Acne Linked to PCOS?
Yes. PCOS increases androgen and insulin levels, leading to breakouts. Managing PCOS helps reduce hormonal acne flare-ups effectively.
Can Men Get Hormonal Acne Too?
Yes, men can also experience it. High testosterone levels can boost oil production, which leads to deep and painful breakouts.
What Are the Best Birth Control Options for Acne?
Combination birth control pills containing estrogen and progestin often work best. Always consult your doctor before choosing one.
Can Diet or Supplements Improve Hormonal Acne?
Yes, a low-sugar, anti-inflammatory diet and supplements like zinc or omega-3s can help get rid of hormonal acne naturally over time.
Are Natural Remedies Enough for Severe Acne?
Natural methods help mild acne, but severe hormonal acne may require medical treatments for the best and safest results.

This article is medically reviewed by Dr. Nivedita Pandey, Senior Gastroenterologist and Hepatologist, ensuring accurate and reliable health information.
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist specializing in pre and post-liver transplant care, as well as managing chronic gastrointestinal disorders. Known for her compassionate and patient-centered approach, Dr. Pandey is dedicated to delivering the highest quality of care to each patient.








