Antibiotics for a tooth infection stop the bacteria that cause pain and swelling. You need them when an infection spreads beyond the tooth or when you have a fever or facial swelling. Antibiotics lower bacteria and ease symptoms, but they do not fix the broken or dead tooth that started the problem. See a dentist for the lasting fix.
What Are Antibiotics for Tooth Infections and How Do They Work?
How Bacterial Infections Develop Inside A Tooth Or Gum
Bacteria enter a tooth through a cavity, crack, or gum disease. They reach the pulp (the soft center with nerves and blood vessels) and multiply. Pus forms and pressure builds. That causes sharp or throbbing pain. If the body cannot stop the bacteria, the infection can spread to nearby tissue or the bloodstream. Early care stops the spread.
The Role Of Antibiotics In Stopping Bacterial Growth
Antibiotics kill or block the growth of bacteria. They travel in your blood to the infected area. When the right antibiotic reaches the germs, swelling and fever fall. Antibiotics are especially helpful if the infection is spreading or you have a weak immune system. Your dentist follows guidelines to pick the best drug and the length of treatment.
Why Antibiotics Alone Do Not Cure The Root Cause Of Infection
Antibiotics cannot remove dead tissue inside a tooth. If a tooth is cracked or the pulp is dead, the infection source remains. You still need dental treatment. A root canal or extraction removes infected tissue. Without that, the infection can come back even after antibiotics drop the symptoms. The medicine is a bridge, not the whole fix.
Best Antibiotic For Tooth Infection
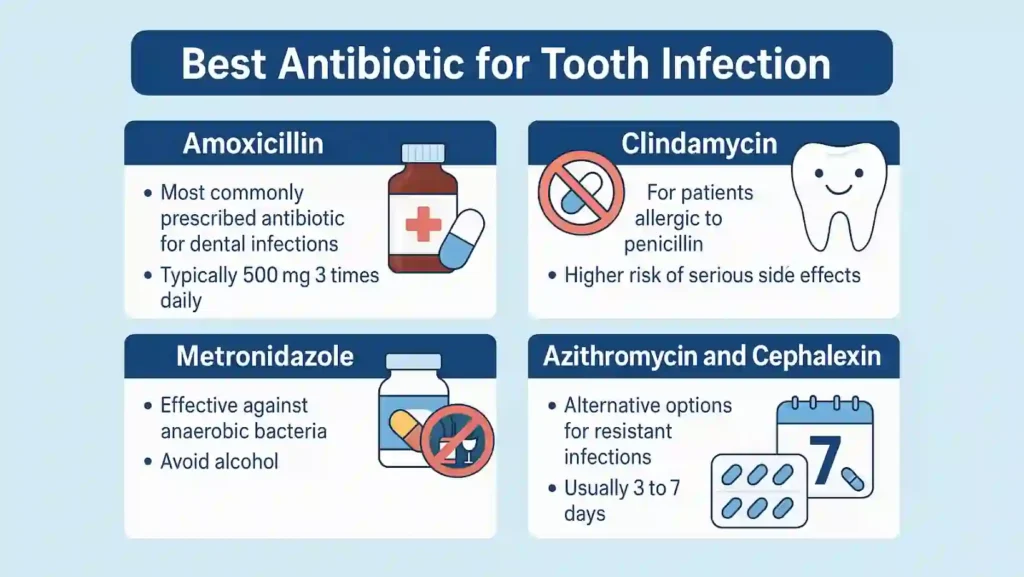
Amoxicillin: The Most Commonly Prescribed Antibiotic For Dental Infections
Your dentist will often choose amoxicillin first. It works on many bacteria that cause tooth infections. Typical adult dosing is 500 mg three times a day for three to seven days, depending on the case. Short high-dose courses are common and effective. Finish every dose. Stopping early risks return and resistance.
Clindamycin: For Patients Allergic To Penicillin
If you are allergic to penicillin, your dentist might pick clindamycin. Clindamycin reaches bone and abscesses well. But it has a higher risk for serious side effects, such as Clostridioides difficile infection (severe diarrhea). Many guidelines now urge caution with clindamycin and suggest other alternatives when possible. Tell your dentist about any drug allergies.
Metronidazole: Effective Against Anaerobic Bacteria
Some oral bacteria do not need oxygen to live (anaerobes). Metronidazole treats these bacteria well. Dentists sometimes combine metronidazole with amoxicillin for tougher infections. Avoid alcohol while using metronidazole. Your dentist will tell you the right dose and duration.
Azithromycin And Cephalexin: Alternative Options For Resistant Infections
When common drugs do not work, or when allergies limit choices, dentists may use azithromycin or cephalexin. These cover different bacterial types. Your dentist chooses based on severity, allergy history, and local resistance patterns. Never switch or stop drugs without guidance.
Duration, Dosage, And Safety Considerations For Common Antibiotics
Most dental infections respond to short courses, often three to seven days. Your clinician may ask you to recheck within 48 to 72 hours. Stop antibiotics 24 hours after your systemic signs resolve, if advised.
Keep pregnant, breastfeeding, and chronic health patients informed before taking antibiotics. Report severe allergies immediately. These safety steps reduce side effects and resistance.
Natural Antibiotics For Tooth Infections
Natural Antibacterial Remedies: Garlic, Clove Oil, And Turmeric
Some natural items have antibacterial and anti-inflammatory properties. Garlic contains allicin. Clove oil contains eugenol, which can numb pain. Turmeric has curcumin, which reduces inflammation.
These items can lower surface bacteria and ease pain for a short time. They are not proven to cure deep tooth infections. Use them only for temporary relief while you get dental care.
Warm Saltwater Rinses And Hydrogen Peroxide Mouthwash
Saltwater rinses reduce swelling and loosen debris. Mix half a teaspoon of salt in eight ounces of warm water. Swish and spit. A diluted 3% hydrogen peroxide rinse mixed half-and-half with water may reduce oral germs. Do not swallow hydrogen peroxide. These rinses are safe, short-term measures to help comfort and hygiene.
Tea Tree Oil And Coconut Oil Pulling: What Research Says
Tea tree oil kills some bacteria in lab tests. It can irritate gums if used undiluted. Coconut oil pulling (swishing oil for 10–20 minutes) may lower surface bacteria and freshen breath. Evidence is limited and mixed. These methods support hygiene but cannot remove infected tissue. Use caution and do not use essential oils undiluted on gums.
When Natural Treatments Can Support — Not Replace — Antibiotics
Natural remedies can ease pain until you see a dentist. They may reduce bacteria on the surface. But they cannot reach bacteria deep in a root canal or abscess. If you have swelling, fever, spreading redness, or trouble breathing, natural care is not enough. Seek urgent dental or medical care. Follow your dentist’s instructions on combining home care with prescribed medicine.
Easiest Way To Get Antibiotics For a Tooth Infection
Getting A Prescription From A Dentist Or Telehealth Provider
The safest and easiest way to get antibiotics for a tooth infection is through a dentist. Dentists can check the source of pain, take an X-ray if needed, and choose the right antibiotic.
If you can’t visit a clinic quickly, a telehealth consultation is another legal option. Online dentists can look at your symptoms, ask questions, and send a valid prescription to your local pharmacy.
Never try to order antibiotics from unverified websites. Many online “pharmacies” sell fake or expired drugs that can cause harm.
Why You Should Avoid Self-Medicating With Leftover Antibiotics
Using leftover or borrowed antibiotics is dangerous. Each drug treats certain bacterial types. Old pills may not match the infection. Taking them for too few days or at low doses can let bacteria survive and grow stronger.
That’s how antibiotic resistance begins, when bacteria no longer respond to drugs that once worked. Always complete a fresh, full course given by a licensed dentist or doctor.
How Online Dental Consultations Provide Legitimate Prescriptions
Tele-dentistry has grown fast. After a video or photo exam, the dentist can prescribe the right antibiotic for a tooth infection if needed.
Most online dental clinics operate under state dental boards and follow the same rules as in-person visits.
They also help you find the nearest emergency room if they suspect a deep abscess or spreading infection. This makes tele-dentistry a safe shortcut when you can’t get to a chair in time.
When Emergency Antibiotics Are Needed For Spreading Infections
If swelling spreads to your cheek, jaw, or neck, you need emergency care. Trouble swallowing, fever above 101°F (38.3°C), or a racing heartbeat mean the infection is spreading.
Go to the emergency room if you can’t reach your dentist. There, you might get IV (intravenous) antibiotics such as penicillin G, ampicillin-sulbactam, or clindamycin if you’re allergic.
Prompt care can stop serious complications like sepsis (blood infection) or Ludwig’s angina (severe swelling under the jaw that can block airways).
How To Make Homemade Antibiotics For Tooth Infection
Why “Homemade Antibiotics” Should Never Replace Prescription Drugs
There is no safe way to produce real antibiotics at home. Drugs like amoxicillin or metronidazole need lab-grade processes and purity checks. Homemade mixes from herbs or food can never reach infection sites inside a tooth.
Still, certain natural care steps can calm pain or swelling while you wait for your dentist. They are support measures, not cures.
Evidence-Based Home Care Options For Mild Tooth Pain
When you can’t see a dentist right away, try:
- Rinsing your mouth with warm saltwater three times daily.
- Applying a cold pack on the outside of the cheek to reduce swelling.
- Taking pain relievers such as ibuprofen or acetaminophen as directed.
- Sleeping with your head slightly raised to ease pressure.
These steps do not replace antibiotics for tooth infection, but they make discomfort more manageable until you get proper care.
Natural Ingredients That Reduce Bacterial Load And Inflammation
Certain household items can slow bacterial growth on the gum surface:
- Clove oil: Dab a drop on cotton and press gently against the sore tooth for temporary numbness.
- Turmeric paste: Mix turmeric powder with a little water to make a paste and apply to the gum for mild anti-inflammatory relief.
- Garlic: Crushed garlic releases allicin, which has antibacterial properties.
These can’t enter the infected pulp, so use them only alongside medical care.
When To Combine Home Remedies With Prescribed Treatment
Your dentist may advise warm salt rinses or clove oil for pain while you take antibiotics. The right combination speeds healing and keeps the mouth clean.
Always tell your dentist about any herbal products you use. Some herbs can interfere with antibiotic absorption. Following your dentist’s full plan gives the best results for clearing infection and preventing relapse.
Symptoms That Indicate You Need Antibiotics For Tooth Infection
Signs Your Infection Is Spreading (Swelling, Fever, Or Pain In The Jaw)
Early tooth infections might feel like dull pressure or mild pain. But if swelling reaches your face, neck, or jaw and you develop fever or chills, the bacteria have likely spread.
Another red flag is swollen lymph nodes (small glands in your neck). They enlarge when the body fights infection. At this stage, only antibiotics for tooth infection can control bacteria, while dental work removes the cause.
How To Tell If Your Tooth Infection Needs Immediate Antibiotics
You need urgent treatment if you notice:
- Throbbing pain that radiates to your ear or neck.
- Fever or general weakness.
- Swelling that makes it hard to open your mouth.
- Bitter taste or pus discharge near the tooth.
All these signs show active bacterial growth inside or around the tooth. Getting the best antibiotic for a tooth infection early can stop deeper tissue damage.
When Home Care Isn’t Enough To Manage Pain Or Swelling
If saltwater rinses or over-the-counter painkillers stop helping after one day, it’s time for a dental visit. Pain lasting longer than 48 hours or swelling that keeps growing means the infection has reached the root or jawbone. Antibiotics and dental drainage are needed right away.
When To Visit The Emergency Room For Dental Abscess Complications
Go to the ER if you have:
- Difficulty breathing or swallowing.
- Rapid swelling that spreads toward your eyes or neck.
- High fever or confusion.
These symptoms suggest the infection is moving into deeper spaces or the bloodstream. IV antibiotics can save your life. Do not delay medical attention.
How Long Do Antibiotics Take To Work For A Tooth Infection?
Expected Timeline For Pain Relief After Starting Antibiotics
Once you start antibiotics for a tooth infection, pain and swelling often begin to ease within 48 to 72 hours. Fever usually drops first, followed by less pressure and better jaw movement.
However, even if symptoms improve, bacteria can remain inside the damaged tooth until it’s repaired or removed. Keep your dental appointment for full recovery.
What To Do If Symptoms Don’t Improve Within 48–72 Hours
If pain, fever, or swelling stay the same after three days of antibiotics, call your dentist. They might switch to another antibiotic for a tooth infection or perform drainage. Never double your dose on your own. Some bacteria may resist the first drug, and your dentist will pick a stronger one, like amoxicillin with metronidazole or azithromycin.
Signs Of Antibiotic Resistance Or Ineffective Treatment
Watch for these warning signs:
- Pain and swelling worsen after initial relief.
- Fever returns after stopping the medicine.
- New swelling develops in another area.
If this happens, your dentist may take a sample of pus to identify the bacteria. That helps choose a more effective antibiotic.
How To Complete Your Full Antibiotic Course Safely
Always finish your full course, even if you feel better. Stopping early can leave some bacteria alive and cause a rebound infection. Take pills at the same time daily. Drink water with each dose. Avoid skipping doses.
If you forget a dose, take it as soon as you remember unless it’s almost time for the next one. Completing the course ensures full healing and prevents antibiotic resistance.
Prevention And Aftercare Tips To Avoid Future Tooth Infections
How Good Oral Hygiene Prevents Bacterial Buildup
- The best protection against infection is daily cleaning. Brush twice a day with fluoride toothpaste.
- Floss between teeth to remove trapped food and plaque.
- Use an antibacterial mouthwash once a day if your dentist recommends it.
Good hygiene limits bacterial growth that can lead to decay and infection.
Foods And Habits That Help Strengthen Gums And Teeth
- Eat foods rich in calcium (like milk, cheese, and yogurt) to strengthen enamel.
- Crunchy fruits and vegetables like apples and carrots scrub plaque away.
- Avoid too much sugar or acidic drinks. They weaken enamel and feed bacteria.
- Do not smoke; tobacco slows healing and increases infection risk.
When To Schedule Dental Cleanings For Prevention
- Visit your dentist every six months for professional cleanings.
- People with gum disease or diabetes may need visits every three to four months.
- Regular checkups catch early decay or cracks before bacteria enter the pulp.
- Early fixes mean no need for antibiotics later.
Importance Of Treating Cavities Early To Avoid Abscess Formation
A small untreated cavity can lead to an abscess. Once bacteria reach the pulp, the infection spreads fast.
Treating cavities early through fillings or crowns prevents this. Dental sealants for kids and fluoride treatments for adults also reduce risk. Prevention costs less pain and money than emergency treatment.
FAQ
Can You Get Antibiotics For a Tooth Infection Without Seeing A Dentist?
You can get antibiotics for a tooth infection only after a dental or telehealth exam. Buying drugs without a prescription is unsafe and may worsen resistance.
How Fast Do Antibiotics Work For Tooth Infections?
Most people feel better within 48 to 72 hours after starting the best antibiotic for tooth infection. If symptoms don’t improve, you may need a stronger drug or a dental procedure.
Are There Natural Antibiotics That Actually Work?
Natural antibiotics for tooth infection, like clove oil, garlic, and turmeric, can help surface pain, but they cannot cure deep infections. Always combine them with dentist-approved treatment.
How Do I Know If My Tooth Infection Is Healing?
Pain, swelling, and fever decrease steadily, and you can chew without discomfort. Keep taking the prescribed medicine until your dentist confirms complete healing.
Can A Tooth Infection Go Away On Its Own?
A tooth infection cannot fully heal without dental care. It may seem better for a few days, but bacteria remain trapped inside and can return stronger.
What Happens If I Don’t Treat My Dental Abscess?
An untreated abscess can spread to your jaw, neck, or bloodstream, causing sepsis. You might need hospital IV antibiotics or surgery if you delay treatment.
Is It Safe To Take Leftover Antibiotics From Another Infection?
No. Leftover pills may not match the current bacteria or dose. Taking them increases the risk of antibiotic resistance and incomplete recovery.
What Are The Side Effects Of Dental Antibiotics?
Common side effects include nausea, diarrhea, and rash. Severe allergic reactions are rare but possible. Always tell your dentist about allergies and other medicines you take.














Leave a Comment