Yes, you may feel lower energy when taking antibiotics. The tiredness may come from the medicine, the infection, or both. You may feel sleepy, weak, or slow to think. This section gives clear reasons and simple actions to help you feel better.
Table of Contents
ToggleAntibiotics Tiredness Side Effect:
Antibiotics fight bacteria. They help your body heal. Still, they can change how you feel. You may notice low energy, sleepiness, or lack of drive. These are common reactions. Use care and watch for other signs like rash or trouble breathing.
How Antibiotics Affect Gut Microbiota and Energy Metabolism
Your gut has many helpful bacteria. These microbes break down food into fuel. Some antibiotics reduce helpful bacteria. That change can lower vitamins and short-chain fats that keep you energized. When gut balance shifts, you make less cellular fuel. This is one way antibiotics make you tired.
Antibiotics also change signals from the gut to the brain. When those signals alter, you may feel sluggish. Gut change can raise mild inflammation. Inflammation uses energy and can cause fatigue. If you have stomach upset or loose stools, gut impact is likely.
The Link Between Infection Recovery and Post-Antibiotic Fatigue
Fighting infection takes energy. Your immune system uses sugar and proteins to heal. Even after bacteria are killed, repair continues. Healing uses resources and makes you feel tired. This is not only the drug. It is also how the body fixes damage. That mixed effect explains why antibiotics make you tired during and after treatment.
You may feel worse before better. Fever, aches, and poor sleep drain energy. After antibiotics stop, recovery can take days or weeks. This stage is called post-infection fatigue. It is common and usually improves with time.
Difference Between Infection-Related Tiredness and Medication Side Effects
Infection tiredness starts early, with fever or chills. Medication side effects often start after the first dose. If tiredness began before medication, the infection likely caused most fatigue. If tiredness rose after starting the medicine, the drug may be the reason. Sometimes, both infection and antibiotics make you tired.
If tiredness comes with dizziness, fainting, or a fast heartbeat, contact a doctor. These signs may mean a bad reaction. Mild sleepiness and slower thinking are more often harmless.
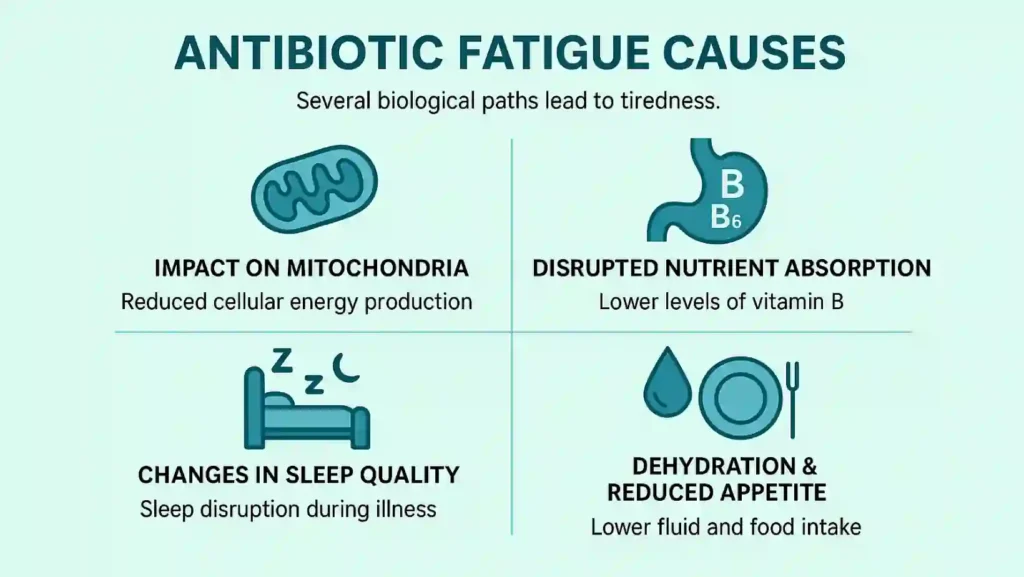
Antibiotic Fatigue Causes:
Several biological paths lead to tiredness. Some relate to cells. Others link to nutrition and sleep.
Impact of Antibiotics on Mitochondria and Cellular Energy
Mitochondria are tiny parts in cells that make energy. Some antibiotics affect mitochondrial function. When mitochondria slow, less ATP (cell fuel) is produced. Low ATP means less strength and more fatigue. This cell-level change explains why antibiotics make you tired for some people.
Not every antibiotic damages mitochondria. The risk depends on the type and dose. People with existing low energy may notice this effect more.
Disruption of Nutrient Absorption and Vitamin B Deficiency
Gut bacteria help release vitamins from food. They support vitamin B production and absorption. Antibiotics can reduce these bacteria. Low B12, B6, or folate can cause tiredness. If you already eat little, this effect grows. This is a clear path showing how antibiotics make you tired.
If you have long-term stomach problems, mention them to your doctor. You may need a blood test for vitamin levels if fatigue lingers.
Changes in Sleep Quality and Immune Recovery During Treatment
Illness often interrupts sleep. Pain, cough, and fever wake you. Some antibiotics can also upset sleep. Poor sleep reduces daytime energy. Your immune system then needs more time to fix the body. That combination makes you feel tired and slow. This is another reason antibiotics make you tired while you recover.
Try to keep a bedtime routine. Good sleep helps the immune system and speeds recovery.
How Dehydration and Reduced Appetite Add to Fatigue
Antibiotics may cause nausea or stomach upset. You might eat less or drink less water. Dehydration reduces blood volume and makes you weak. Low food intake lowers energy stores. These are simple causes of tiredness. Together, they show why antibiotics make you tired when you do not eat or drink enough.
Drink small amounts often. Choose easy foods like soups, fruit, and yogurt to keep energy steady.
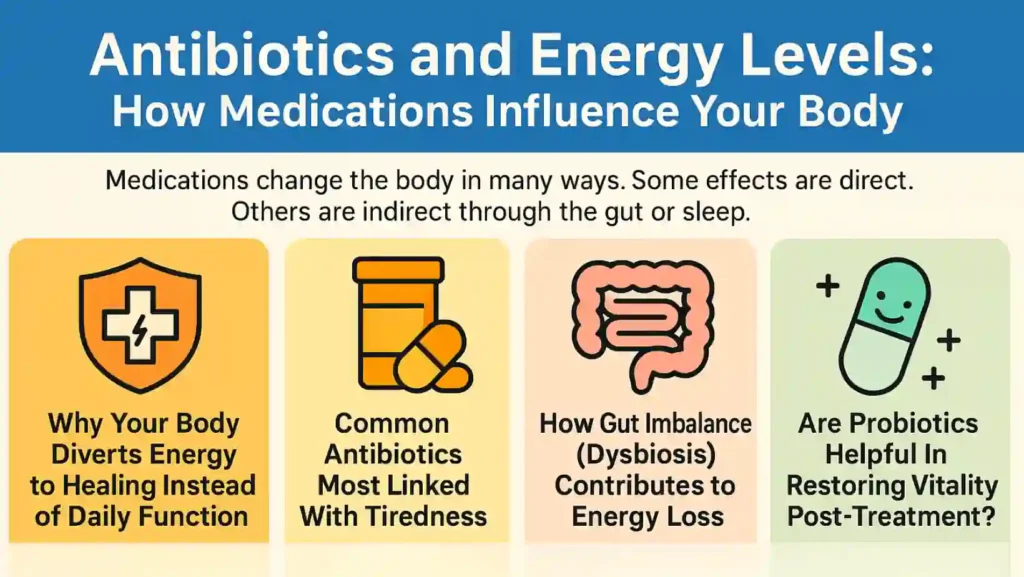
Antibiotics and Energy Levels: How Medications Influence Your Body
Medications change the body in many ways. Some effects are direct. Others are indirect through the gut or sleep.
Why Your Body Diverts Energy to Healing Instead of Daily Function
When you are sick, the body shifts energy to immune tasks. White blood cells, fever, and tissue repair use fuel. That leaves less energy for work, thinking, and play. This normal shift explains why antibiotics make you tired while you fight an infection. It is not laziness. It is how the body prioritizes repair.
Common Antibiotics Most Linked With Tiredness
Some commonly used antibiotics have more reports of fatigue. These include amoxicillin and doxycycline. Fluoroquinolones can cause strong side effects in some people. Not everyone will feel tired. If your drug causes heavy sleepiness, tell your prescriber. They may offer a switch.
Reports link tiredness to gut and cell effects. The dose and length of treatment also matter. Short courses often cause less fatigue than long ones.
How Gut Imbalance (Dysbiosis) Contributes to Energy Loss
Dysbiosis means an unstable gut community. It lowers digestion and vitamin supply. It may increase gut inflammation. That inflammation sends signals to the brain. These signals cause low mood and low drive. Dysbiosis is a main reason antibiotics make you tired for days after treatment ends.
Eating fiber and fermented foods helps the gut community rebuild. A balanced gut supports steady energy and clearer thinking.
Are Probiotics Helpful in Restoring Vitality Post-Treatment?
Probiotics are live bacteria that can help the gut. Some studies show they reduce diarrhea and restore balance after antibiotics. For energy, probiotics can help indirectly by fixing digestion and vitamin production. They do not guarantee instant energy, but they often speed recovery.
Choose a probiotic with proven strains. Talk to your provider before starting any supplement. This can help reduce how long antibiotics make you tired after treatment ends.
Why Am I Tired While On Antibiotics?
Feeling worn out during treatment can be confusing. You start taking medicine to feel better, yet you end up more tired. Knowing what’s normal and what needs attention can help you handle it better. There are many reasons why antibiotics make you tired, but most are temporary and harmless.
Normal Short-Term Tiredness During Antibiotic Therapy
It’s normal to feel extra tired while taking antibiotics. Your body is fighting off infection while adjusting to strong medicine. You may feel sleepy, foggy, or heavy-limbed. This usually fades once the infection clears and the drug course ends. The tiredness is your body’s way of saying it needs more rest to heal. So yes, antibiotics make you tired, but this is often short-lived.
If you sleep more than usual or feel like you can’t get out of bed, that’s your body using energy to heal tissues damaged by infection. It’s not weakness; it’s recovery in progress.
When Fatigue Signals an Allergic or Adverse Reaction
Sometimes tiredness isn’t simple. If your fatigue comes with symptoms like rash, swelling, dizziness, or shortness of breath, it could be an allergic reaction. Severe weakness with these signs means you should stop taking the medicine and call a doctor immediately.
This rare but serious condition is different from normal tiredness. Here, antibiotics make you tired because your immune system is reacting against the drug itself.
When To Consult A Doctor About Persistent Exhaustion
If you finish your medication and still feel weak for weeks, don’t ignore it. Your doctor may test for vitamin loss, dehydration, or infection relapse. Persistent tiredness might not be just because antibiotics make you tired. It can also point to anemia, thyroid problems, or lingering infection. A medical check ensures that nothing serious is hiding behind fatigue.
Other Medications That May Intensify Antibiotic Fatigue
If you’re taking painkillers, antihistamines, or antidepressants, the combination may make you sleepier. Some blood pressure drugs and anti-anxiety medicines can worsen fatigue, too. These interactions can make it feel like antibiotics make you tired more than usual.
Always tell your doctor about all the medicines and supplements you take so they can adjust your plan safely.
Antibiotics Fatigue Recovery: Regaining Strength After Treatment
When your course is done, the body slowly resets. The gut microbiome rebuilds. The immune system calms down. But getting your energy back takes care. This recovery phase is key to reducing post-treatment exhaustion.
How To Restore Gut Health And Energy Balance Post-Antibiotics
Once you finish antibiotics, rebuild your gut health. Your gut bacteria help control digestion, energy, and immunity. When they’re out of balance, you feel drained.
Here’s what helps:
- Eat fermented foods like yogurt, kefir, kimchi, or sauerkraut.
- Include fiber-rich fruits, vegetables, and whole grains to feed good bacteria.
- Take probiotics if your doctor approves them.
Restoring your gut helps you process nutrients better. That alone can reduce how much antibiotics make tired you get after treatment.
Importance Of Hydration, Sleep, And Light Physical Activity
Water, rest, and movement are simple but powerful recovery tools. Dehydration thickens blood and lowers circulation, making you sluggish. Proper sleep allows cell repair and hormone balance. Light activity like walking increases oxygen flow, helping your body regain rhythm. These habits work together to limit the time antibiotics make you tired.
Nutrients That Boost Recovery (Probiotics, B Vitamins, Magnesium)
Nutrients play a large role in regaining energy.
- B vitamins restore brain and nerve function.
- Magnesium relaxes muscles and improves sleep.
- Probiotics help your gut absorb vitamins again.
Include eggs, meat, fish, dairy, leafy greens, nuts, and seeds. If needed, take supplements after medical advice. These nutrients address one of the biggest antibiotic fatigue, nutritional imbalance.
Timeline: How Long Fatigue Lasts After Stopping Antibiotics
Most people regain strength within one to three weeks. If you had a serious infection, it might take longer. The gut bacteria need time to repopulate, and mitochondria recover gradually. For most, tiredness peaks during the last few days of treatment and fades soon after. But remember, the recovery time can vary based on health and diet. That’s why it’s hard to set a single timeline for how long antibiotics make you tired.
Additional Factors That May Make You Feel Tired During Antibiotic Use
Tiredness doesn’t always come from the medicine alone. Sometimes other factors combine with antibiotics to make you feel worse.
Concurrent Illness Or Immune Response To Infection
Even if antibiotics are working, your immune system may still be active. White blood cells release chemicals to clean up infection, which can trigger fatigue. The immune response itself explains why antibiotics make you tired even when the infection is nearly gone.
Poor Diet Or Caloric Restriction While Unwell
During illness, appetite often drops. When you eat less, you get fewer calories and less protein for repair. That starves your muscles and brain of energy. Eating easy-to-digest, nutrient-rich meals can help balance this effect. Skipping meals can make it feel like antibiotics make you tired more than they actually do.
Underlying Conditions That Worsen Fatigue (Thyroid, Anemia, Etc.)
If you have thyroid imbalance, anemia, diabetes, or chronic fatigue syndrome, antibiotics can amplify tiredness. These conditions already have lower energy levels. When you add antibiotics, your system slows even more. Identifying and treating these issues can reduce the feeling that antibiotics make you tired every time you take them.
Psychological Fatigue Due To Prolonged Illness Or Medication Stress
Being sick is stressful. Constant worry, poor sleep, and the burden of medication can wear you down. Mental fatigue often feels just like physical exhaustion. This mental stress is another reason why antibiotics make you tired even when tests show you’re improving.
Tips To Manage Antibiotic-Related Fatigue Safely
You can’t always avoid fatigue, but you can manage it. These simple actions help you recover faster while keeping treatment safe.
How To Balance Rest And Movement During Treatment
Rest when your body asks for it. Don’t force hard exercise during infection. But too much bed rest can make muscles weak. Gentle stretching or slow walking boosts circulation and mood. This balanced approach helps minimize how much antibiotics make you tired during recovery.
What Foods To Eat To Maintain Energy Levels
Choose easy, nourishing meals:
- Lean proteins: chicken, eggs, beans
- Whole carbs: brown rice, oats, potatoes
- Fruits and veggies: provide vitamins and fiber
- Yogurt: for probiotics
Avoid greasy and sugary foods that cause energy crashes. A balanced diet can cut down on antibiotic fatigue and restore steady energy.
When To Take Antibiotics (Morning Vs Night) To Minimize Drowsiness
If your antibiotic causes sleepiness, take it at night. If it causes nausea, take it with breakfast. Timing can affect how antibiotics make you tired throughout the day. Always follow label instructions or your doctor’s advice about timing and food.
Supplements That Help Restore Gut And Energy Balance
Supplements can fill the gap between meals and full recovery.
- Probiotics: restore gut flora
- Vitamin B complex: boosts energy
- Magnesium: reduces stress and improves sleep
Take only what your doctor recommends. Overdoing supplements can upset digestion and make recovery slower. Used wisely, they can help shorten how long antibiotics make you tired.
FAQ
Do All Antibiotics Make You Tired?
Not all, but many can. The effect depends on the drug, your body, and the infection. Some antibiotics change gut bacteria or cell energy more than others, which explains why antibiotics make you tired.
How Long Does Antibiotic Fatigue Last?
It can last from a few days to a few weeks. For most people, it fades within two weeks after stopping the medicine. Duration depends on infection type and rest level.
Can Probiotics Reduce Tiredness During Antibiotics?
Yes, probiotics can help. They restore gut bacteria and improve nutrient absorption. Taking them may lessen how much antibiotics make you tired during and after treatment.
Is Feeling Weak While Taking Antibiotics Normal?
Yes, mild weakness is normal. Your body diverts energy to healing. Drink fluids, rest, and eat well. But call a doctor if weakness becomes extreme or constant.
Should I Stop Taking Antibiotics If I Feel Too Tired?
No, don’t stop without medical advice. Incomplete treatment can let infection return. Contact your doctor for guidance. They may adjust your dose or timing.
Which Antibiotics Are Most Likely To Cause Fatigue?
Drugs like amoxicillin, doxycycline, and ciprofloxacin are often linked with tiredness. They may affect the gut or cell energy. But not everyone reacts the same way.
Can Antibiotic Fatigue Be Confused With Post-Infection Fatigue?
Yes. After infection, the body still repairs cells and tissues, which causes similar tiredness. Doctors can help tell whether your fatigue is from infection or medication.
Does Antibiotic Use Affect Energy Recovery After Illness?
Yes, antibiotics can slow recovery by altering gut balance. But they also remove infection, which helps long-term energy return. Proper diet and hydration help speed this up.

This article is medically reviewed by Dr. Nivedita Pandey, Senior Gastroenterologist and Hepatologist, ensuring accurate and reliable health information.
Dr. Nivedita Pandey is a U.S.-trained gastroenterologist specializing in pre and post-liver transplant care, as well as managing chronic gastrointestinal disorders. Known for her compassionate and patient-centered approach, Dr. Pandey is dedicated to delivering the highest quality of care to each patient.