What Are Autoimmune Diseases?
Autoimmune diseases occur when the immune system, which normally fights off infections, mistakenly attacks the body’s own tissues. This is referred to as an immune-mediated disorder.
Your body can no longer tell the difference between foreign invaders and its own healthy cells. Many of these are chronic inflammatory diseases because the body stays inflamed for long periods.
So what is autoimmune disease? It’s when your overactive immune system, causing inflammation symptoms like heat, swelling, and pain, even when there’s no sign of germ attack.
Types of Autoimmune Diseases
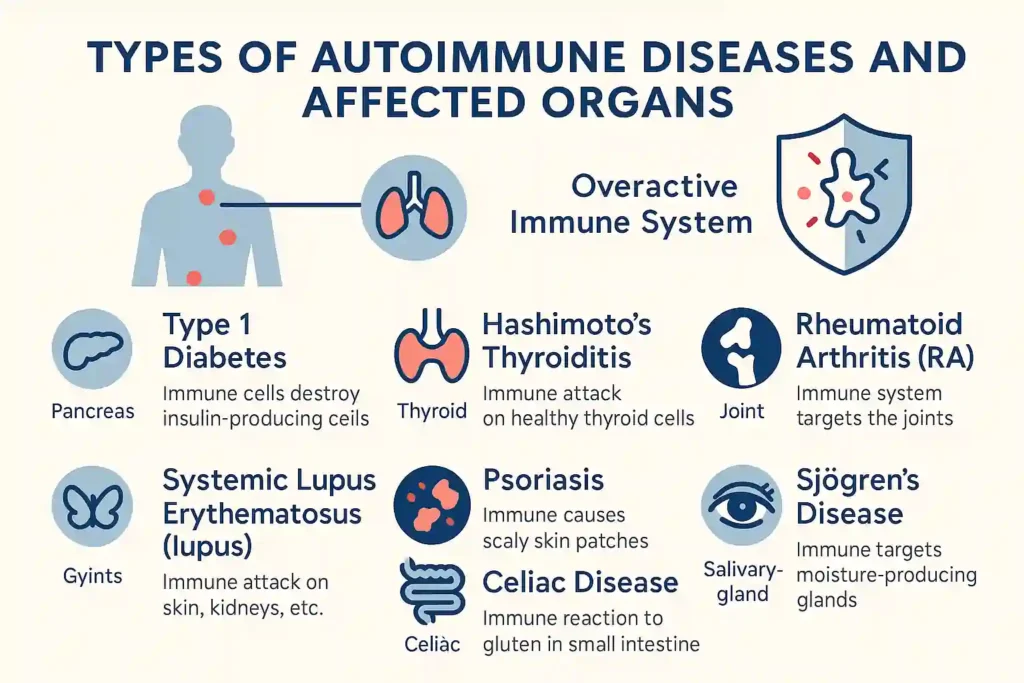
Autoimmune disorders are classified into more than 80 categories. Each type affects different organs or tissues in the body. Some are widespread, while others target a single organ.
A few examples from the autoimmune disease list include:
- Type 1 diabetes: The immune system damages insulin-making cells in the pancreas. People feel very thirsty, pee a lot, and lose weight
- Hashimoto’s thyroiditis: It attacks the thyroid, slowing it. That causes tiredness, weight gain, feeling cold, and hair loss.
- Multiple sclerosis (MS): The immune system damages nerves. Symptoms include feeling weak, numb, blurry vision, poor coordination.
- Rheumatoid arthritis (RA): The immune system attacks joints. They get swollen, stiff, and painful. It may affect lungs or eyes too.
- Systemic lupus erythematosus (lupus): A serious one affecting skin, kidneys, heart, lungs. Causes rashes, joint pain, fever, fatigue.
- Psoriasis: Skin immune attack causes itchy red patches. Sometimes it also affects joints as psoriatic arthritis.
- Celiac disease: A reaction to gluten; the immune system damages the small intestine leading to tummy pain, diarrhea, anemia.
- Sjogren’s disease: Causes dry eyes and mouth, joint pain, fatigue, brain fog.
How Common Are Autoimmune Diseases?
Autoimmune diseases are more prevalent than many individuals realize. Experts estimate that approximately one in 15 people in the U.S. is affected.
Women are more likely to get them than men. They often start during the childbearing years but can appear at any age. Often people can have more than one autoimmune disease called multiple autoimmune syndrome, where one immune attack leads to others.
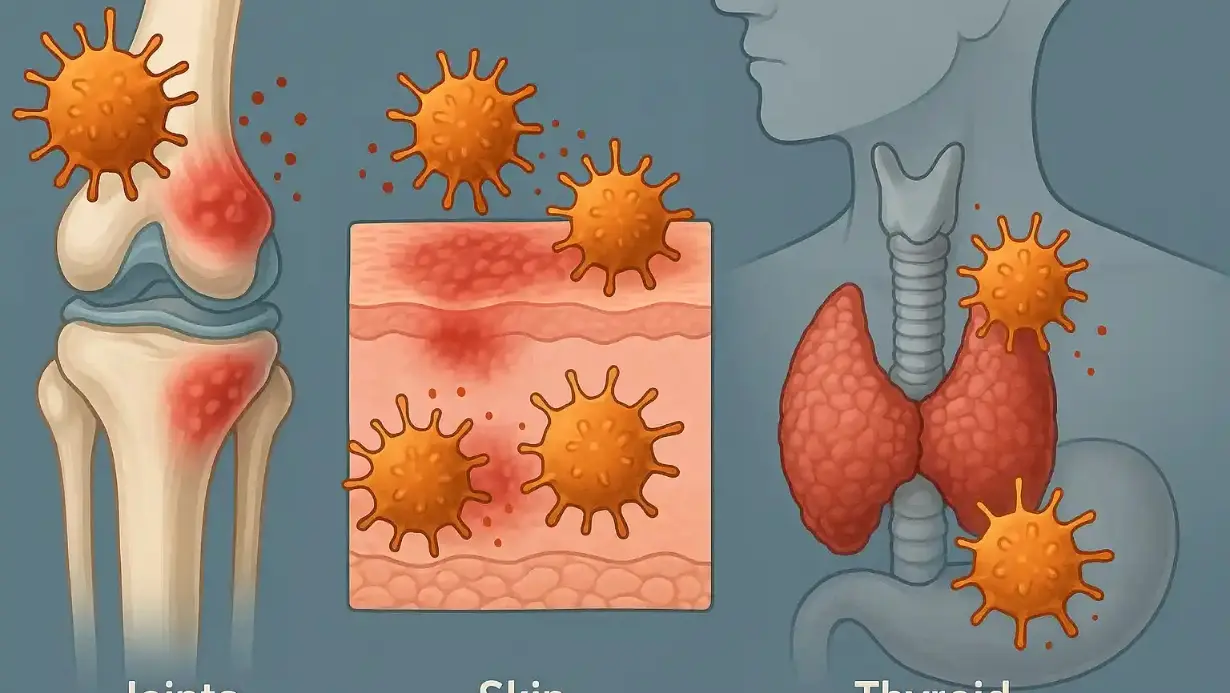
Symptoms of Autoimmune Diseases

The symptoms of autoimmune disease vary, but many share common ones:
- Extreme fatigue
- Joint pain and swelling
- Skin rashes or irritation
- Digestive troubles like stomach pain or diarrhea
- Recurring low fevers
- Swollen glands
These signs of autoimmune disease can come and go. Sometimes they’re mild. Other times, they flare up and become serious.
Causes and Risk Factors of Autoimmune Diseases
Doctors do not fully know why common autoimmune diseases appear. However, it is believed that genetics and various triggers contribute to the onset of these diseases. Some known risk factors:
- Family history (some genes raise risk)
- Viral infections (like Epstein‑Barr virus) Wikipedia
- Smoking, obesity, toxin exposure NIEHSwebmd.com
- Having one autoimmune disease makes others more likely
These risk factors together may tip the balance into autoimmunity.
How Autoimmune Diseases Are Diagnosed
Doctors first ask about symptoms and health history. They examine you and may order tests such as:
- Blood tests that look for autoantibodies like ANA (antinuclear antibody) test
- Markers of inflammation
- Imaging tests like X‑rays, MRI
- Sometimes a tissue biopsy for deeper look
Diagnosis can be hard. Many diseases share symptoms, so doctors rule out other causes before saying it’s an autoimmune condition.
Treatment Options for Autoimmune Diseases
Currently, there is no cure for most. However, the goal of treating autoimmune diseases is to regulate immune function and symptoms:
- Medicines like corticosteroids ease swelling fast
- NSAIDs reduce pain and inflammation
- Immunosuppressants slow the immune attack (e.g. methotrexate, azathioprine)
- Biologics target specific immune chemicals like TNF or interleukin—safer for long-term use
- Disease-specific treatments: insulin for type 1 diabetes, hormone replacement in thyroid cases, gluten‑free diet in celiac disease
- Physical therapy or Autoimmune-safe exercise like walking or water aerobics helps mobility
Exciting research includes inverse vaccines that may teach the immune system to tolerate specific targets rather than suppress everything. Trials are ongoing for MS, celiac disease, lupus, with hope for approval in 5–10 years
Living With an Autoimmune Disease
Living well with an autoimmune condition depends on:
- Following doctor’s plan and regular check‑ups
- Eating a balanced diet and reducing stress
- Using Healthy immune function habits: sleep, exercise, avoid smoking
- Joining support groups or therapy to manage emotional challenges
Even with challenges, most people can lead full lives.
Can Autoimmune Diseases Be Cured?
Most cannot be fully cured today. Instead, treatments help control the disease and manage flares. However, it’s possible to live symptom‑free for long periods. A few conditions improve with early action. And new treatments like inverse vaccines may one day offer cures.
Life Expectancy and Prognosis
Focusing on control, many people with autoimmune conditions live normal lifespans. Life expectancy depends on the type and how severe it is. Early diagnosis and treatment improve outcomes.
Preventing Autoimmune Diseases
Autoimmune disorders cannot be prevented with certainty. But some steps may help reduce risk:
- Lower stress
- Eat anti-inflammatory foods, avoid sugar or gluten if sensitive
- Add supplements like vitamin D, omega‑3 under guidance
- Avoid toxin exposure, quit smoking
- Maintain a healthy immune system by engaging in autoimmune-safe exercise.
When to See a Healthcare Provider
Talk to a doctor if you notice signs of autoimmune disease like:
- Persistent fatigue, joint pain, or swelling
- Digestive issues without a clear cause
- Rashes that won’t go away
- Unexpected fevers or weight changes
- Dry mouth or eyes
- Brain fog or nerve issues
Early medical help is important. Keep notes of when symptoms start, what makes them worse or better.
Questions to Ask Your Doctor
- What autoimmune diseases might match my symptoms?
- What tests will you run?
- What treatment do you recommend—medicines, diet, exercise?
- What side effects can I expect from the medicines?
- Can I reduce risk of other autoimmune diseases?
- How often should I follow up?
Discussing openly helps you stay informed and confident.
Encouragement and Final Note
Dealing with autoimmune diseases can feel scary. But you are not alone. Many people manage these conditions well. With medicine, exercise, a good diet, and stress care, you can keep flares low and live strong.
New treatments on the way give hope for better control, maybe one day even cures. Focus on what helps you feel better. Your doctor, your team, and your support system are ready to help.
Autoimmune Diseases FAQs
Is autoimmune disease curable?
Most are not yet curable. Treatments control the immune activity and ease symptoms.
What is the most common autoimmune disease?
Some of the common autoimmune diseases include rheumatoid arthritis, psoriasis, lupus, MS, type 1 diabetes, and Hashimoto’s thyroiditis
Can you live a normal life with autoimmune disease?
Yes. With treatment and lifestyle care, many people live full, healthy lives.
What is the cause of autoimmune disease?
There’s no one cause. It often uses a mix of genetics, infections, environment, and immune system issues.
Who usually gets autoimmune disease?
Women are most often affected. Having another autoimmune condition or a family history raises risk.
What is the best medicine for autoimmune disease?
It varies. Options include anti-inflammatories, immunosuppressants, biologics, or disease-specific treatments like insulin or thyroid hormone.
How to test for autoimmune disease?
Tests include blood for autoantibodies, inflammatory markers, imaging or biopsy as needed, plus doctor exam and health history.
Can stress cause autoimmune disease?
Stress may trigger or worsen symptoms, though it doesn’t directly cause autoimmune disease.
At which age does autoimmune disease start?
They can start at any age, from childhood to older adulthood but many begin in teens to mid‑40s.
What are the seven autoimmune diseases?
There isn’t a fixed list, but often referred to are type 1 diabetes, lupus, rheumatoid arthritis, MS, celiac disease, psoriasis, and Crohn’s disease or IBD.
How to heal autoimmune naturally?
Natural steps include a healthy anti‑inflammatory diet, reducing stress, regular gentle exercise, quality sleep, and avoiding smoking. Always do this with doctor’s advice.
What are the signs of autoimmune disease?
Key signs: fatigue, joint pain/swelling, rashes, digestive issues, fevers, dry eyes/mouth, brain fog, weight changes.
Who is most at risk for autoimmune diseases?
People assigned female at birth (especially ages 15‑44), those with family history, and people with another autoimmune disease.













Leave a Comment