Arterial ulcers form when arteries fail to deliver enough blood to the skin. Venous ulcers form when veins fail to pull blood back to the heart. You must know which type you have. The cause decides the tests and the treatment. Correct diagnosis speeds healing and prevents harm.
What’s the Difference Between Arterial and Venous Ulcers?
Overview Of Both Ulcer Types
You see both ulcer types on the lower leg. They are open wounds that heal poorly. Each type has a different cause and shape. Arterial ulcers often come from blocked arteries. venous ulcers come from damaged vein valves and high pressure in the veins. Knowing the difference helps you find the right care.
Underlying Cause: Poor Arterial Blood Flow Vs Venous Reflux
With arterial ulcers, plaque narrows the arteries. Less blood reaches the skin and tissue. Cells die from low oxygen. Peripheral artery disease causes most arterial ulcers. Smoking, diabetes, high cholesterol, and high blood pressure increase risk.
With venous ulcers, vein valves fail. Blood pools in the lower leg. High pressure damages skin and tissues over time. Deep vein thrombosis and long-standing standing raise this risk. Varicose veins often appear first.
Typical Wound Location And Appearance
You can often tell the type by where the wound sits and how it looks.
- Arterial ulcers usually sit on the toes, heels, or the outer lower leg. They look small, deep, and have clean, punched-out edges. The area may be dry and pale. The wound often hurts a lot.
- Venous ulcers usually sit near the inner ankle, in the gaiter area (the lower leg above the ankle). They look wide and shallow. Edges are irregular. The wound often stays moist and has surrounding dark brown skin from long-term swelling.
How Each Type Affects Healing And Tissue Oxygenation
Healing needs oxygen and nutrients. Arterial ulcers have a poor oxygen supply. Low oxygen stops new tissue from forming. These wounds heal slowly or not at all unless blood flow improves.
Venous ulcers get enough oxygen but suffer from fluid buildup and inflammation. The constant swelling stops normal repair. Compression and reducing pressure help healing.
Arterial Vs Venous Leg Ulcer Causes
Causes Of Arterial Ulcers — Poor Blood Supply, Atherosclerosis, Smoking
Arterial causes are linked to blocked or narrowed arteries. The main driver is atherosclerosis (plaque build-up). Smoking speeds plaque growth. Diabetes damages small vessels. High blood pressure and high cholesterol increase plaque risk.
Trauma to a poorly perfused area can trigger an arterial ulcer. If you smoke or have diabetes, your risk rises sharply. Key points you can act on now:
- Quit smoking to slow artery damage.
- Control blood sugar if you have diabetes.
- Treat high blood pressure and high cholesterol.
Causes of Venous Ulcers — Vein Valve Dysfunction, Prolonged Standing, DVT
Venous leg ulcer causes center on valve failure in leg veins. Valves stop blood from flowing backward. When valves fail, blood pools. That raises pressure in small capillaries. Skin breaks down slowly under this pressure. Long periods of standing or sitting and past deep vein thrombosis cause valve damage. Obesity and pregnancy also raise the risk.
Practical steps to lower risk:
- Move often if you must stand or sit for long.
- Use exercise to strengthen your calf muscle pump.
- Seek care for varicose veins or DVT history.
Risk Factors Common To Both Types
Some things raise the chance of either ulcer type. These include:
- Age.
- Obesity.
- Smoking.
- Diabetes.
- Reduced mobility.
If you have any of these, check your legs often.
Lifestyle Habits That Worsen Circulation
You affect healing with daily habits. Smoking harms the arteries quickly. Sitting all day weakens your calf muscle pump. High salt intake worsens swelling. Poor foot care lets small injuries grow. Change these habits to help any leg wound heal.
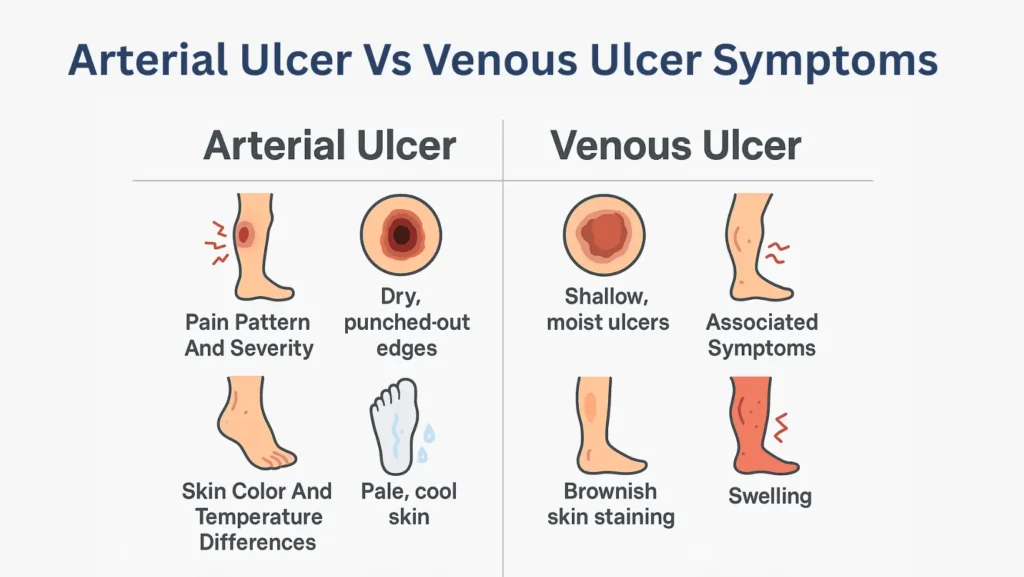
Arterial Ulcer Vs Venous Ulcer Symptoms
Pain Pattern And Severity — Arterial Ulcers Cause Severe Pain, Venous Ulcers Cause Dull Ache
You will notice pain differences. Arterial ulcers cause strong, sharp pain. Pain often increases at night or when you raise the leg. Venous ulcers cause a heavy, aching pain. Elevating the leg usually eases the ache from venous causes.
Wound Appearance — Dry, Punched-Out Edges Vs Shallow, Moist Ulcers
Look at the wound. Arterial ulcers are deep and dry most time. They have a clear, round edge like a punched hole. Venous ulcers are wide, shallow, and wet. They often have yellow or red tissue inside and scaly skin around.
Skin Color And Temperature Differences
Skin near arterial ulcers can look pale or blue. The foot may feel cold. Skin may lose hair. Venous ulcers show brownish skin staining. The area can feel warm and swollen. These signs give strong clues about the cause.
Associated Symptoms — Swelling, Shiny Skin, Or Discoloration
Chronic swelling suggests venous disease. Thin, shiny skin suggests poor arterial flow. If you see redness that spreads, report it. Infection can start quickly in both ulcer types.
How To Clinically Distinguish The Two Ulcer Types
A clinician uses simple tests and exam steps. They check pulses at your ankle and foot. They measure the ankle-brachial index (ABI). ABI compares blood pressure at the ankle with arm pressure. ABI below 0.90 suggests arterial disease. Ultrasound (Doppler or duplex) checks blood flow and valve function. These tests guide safe choices, like whether to use compression.
Arterial Ulcer Vs Venous Ulcer Signs
Arterial Ulcer Signs. Cold Feet, Pale Or Blue Skin, Hair Loss
You can spot many clues just by looking at the leg. Arterial ulcers come with cold skin because little blood reaches the foot. The skin may look pale or even blue. Hair often falls out on the lower leg and toes. Toenails can turn thick and brittle. When you press the skin, it may take a long time to turn pink again. These signs point to poor arterial flow.
Venous Ulcer Signs. Brown Pigmentation, Varicose Veins, Ankle Edema
Venous ulcers come with warm skin and swelling. You may see brown spots around the inner ankle. This happens because iron from old blood leaks into the skin. Varicose veins often sit nearby. Ankle swelling grows as the day goes on. When you press the swollen area, you may see a pit that stays for a few seconds. These are classic venous ulcer signs and help separate venous disease from arterial disease.
Diagnostic Imaging And Vascular Testing (ABI, Doppler, Duplex Scan)
Testing confirms what the exam suggests. ABI checks pressure at the ankle and compares it to the arm. An ABI below 0.90 means poor arterial flow. A handheld Doppler tool helps clinicians find pulses and flow speed. A duplex scan shows how blood moves in the veins and if the valves leak. These tests help decide if the wound is from arterial ulcers or venous ulcers and guide safe treatment plans.
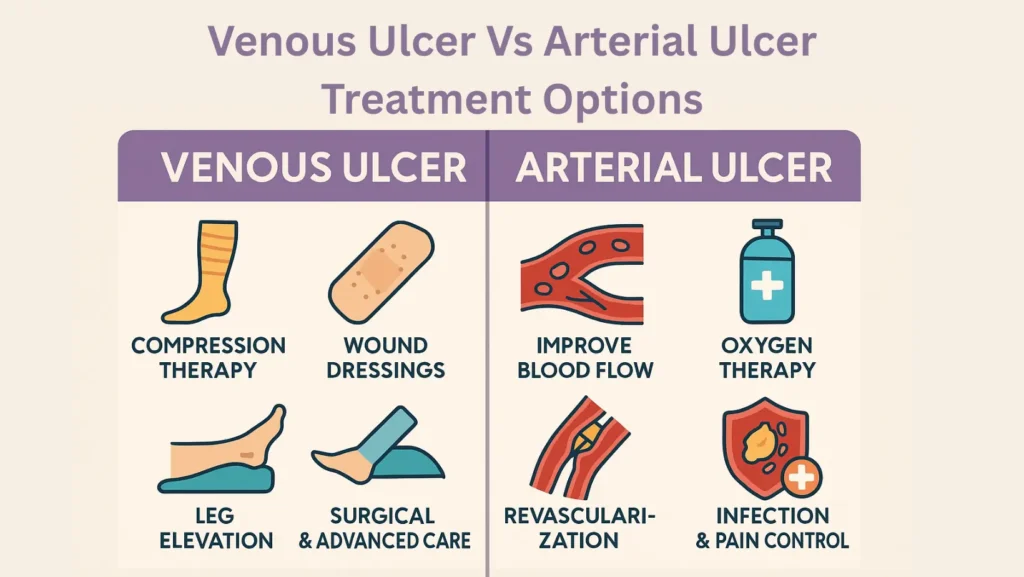
Venous Ulcer Vs Arterial Ulcer Treatment Options
Treating Arterial Ulcers. Improving Blood Flow, Revascularization, Oxygen Therapy
The first goal for arterial ulcers is to improve blood flow. No treatment works if blood flow stays low. A clinician may suggest medicines that reduce clotting or improve circulation. Some people need revascularization. This means opening the blocked artery with a balloon or placing a stent. Others may need bypass surgery, where a new pathway routes blood around the blockage.
In some cases, oxygen therapy helps tissue grow by raising available oxygen. These steps give the wound a chance to form new tissue. Good foot care is also needed because small injuries can turn into large ulcers when blood flow is low.
Treating Venous Ulcers. Compression Therapy, Wound Dressing, Leg Elevation
The main treatment for venous ulcers is compression. Compression reduces swelling and drops vein pressure. This gives the skin a chance to repair. You may use compression wraps or stockings. They must fit correctly to work. Wound dressings keep the ulcer moist but clean. Leg elevation also helps because it pulls fluid out of the lower leg.
For some people, there is a need to treat varicose veins through surgery or vein closure. This lowers the chance of another venous ulcer. These steps create the core plan for venous ulcer and arterial ulcer treatment and show how the two differ in care.
Surgical And Advanced Wound Care Options
Some ulcers need extra help. Skin grafts cover large areas where tissue is missing. Special dressings with growth factors help cells build new layers. For arteries, revascularization stands as the most important step. For veins, closing damaged veins prevents pooling. Each path aims to fix the root cause so the wound can close.
Importance Of Infection Control And Pain Management
Any ulcer can get infected. Infection slows healing and can spread deeper. Signs include warmth, pus, redness, and fever. A clinician may use antibiotics or adjust dressings. Pain control matters too. Arterial ulcers often bring strong pain because nerves lack oxygen. Good pain control helps you move better, which supports circulation.
When To See A Vascular Specialist
You should see a vascular specialist when your wound does not improve in two to four weeks. You should also seek help when pain increases or when you see signs of blocked arteries, like cold toes or color changes. A specialist can perform tests, suggest surgery when needed, and guide safe use of compression.
Healing Outlook. Arterial Vs Venous Ulcers
Healing Timeline And Recurrence Risk
Healing depends on the cause and how quickly treatment starts. Venous ulcers often heal in a few months when compression is used every day. Arterial ulcers take longer because the blood supply must improve first.
Without enough flow, the wound stays open. Recurrence also differs. Venous ulcers can return if swelling or valve problems continue. Arterial ulcers return when plaque buildup grows or if smoking continues.
Why Arterial Ulcers Take Longer To Heal
Blood brings oxygen. Oxygen builds new tissue. Arterial ulcers heal slowly because blocked arteries limit oxygen delivery. Even with the best dressings, the wound will not heal until the flow improves. This is why ABI testing and artery repair often come before any other care.
Preventive Strategies. Lifestyle, Medication, And Early Intervention
Prevention protects you from both ulcer types. Manage diabetes well. Keep cholesterol under control. Take medicines that your clinician prescribes to protect arteries or veins. Address varicose veins when they cause pain or skin changes. Early care for small sores prevents larger wounds from forming.
Role Of Diet, Exercise, And Smoking Cessation
Diet affects circulation. A diet rich in vegetables, lean protein, and healthy fats supports skin repair. Exercise moves blood through the calf pump and protects against swelling. Quitting smoking protects the arteries.
Even one cigarette can shrink arteries and slow healing for hours. Ending tobacco use is the most powerful step for reducing arterial causes and lowering risk for arterial ulcers.
Prevention And Self-Care Tips For Leg Ulcers
Daily Habits To Improve Circulation
Move often. Walking makes the calf muscles squeeze veins and push blood upward. Avoid long sitting or standing. Change positions every thirty minutes when you can. These steps help both arterial ulcers and venous ulcers heal faster and reduce new ulcers.
Foot And Skin Care For Ulcer Prevention
Check your feet each night. Look for red spots or cuts. Wash with mild soap and warm water. Dry well. Use a gentle moisturizer, but skip the space between toes. Wear shoes that fit well to prevent injury.
Wearing Compression Stockings Safely
Compression stockings help people with venous ulcers control pressure and swelling. They must match your leg size. They should not roll down or cut into the skin. Never use strong compression when you have low ABI.
Low ABI means poor arterial flow. Compression in that case can harm the leg. This is why testing is required before using compression for any leg wound.
Reducing Risk Factors For Re Ulceration
You can limit the chance of another ulcer. Keep weight in a healthy range. Control blood sugar. Wear compression daily if you have venous disease. Stop smoking if you have arterial disease. Treat each new scratch early before it becomes a larger wound.
Complications And When To Seek Medical Help
Signs Of Infection And Poor Healing
Signs include more redness, foul smell, warmth, pus, and fever. If the wound grows instead of shrinking, get help quickly. Infection can move to deeper layers or even the bone.
When An Ulcer May Indicate Peripheral Artery Disease (PAD)
A wound that appears on the toes or outer lower leg may point to PAD. Cold feet and weak pulses support this. PAD raises the risk of heart problems. Early diagnosis protects your health and helps the ulcer close.
When Surgery Or Specialist Referral Is Needed
You may need to see a specialist if compression fails for a venous ulcer or if blood flow stays low for an arterial ulcer. Surgery helps restore circulation or fix valve issues. Early referral lowers the risk of limb loss.
Emergency Symptoms To Watch For
Seek emergency care when the foot turns blue or black or loses feeling. Severe pain that appears suddenly can signal artery blockage. Fast help protects tissue.
FAQs
What Is The Main Difference Between Arterial And Venous Ulcers?
The main difference between arterial and venous ulcers comes from the cause. Arterial wounds start when arteries fail to deliver blood. Venous wounds start when veins fail to return blood.
Which Is More Painful? Arterial Or Venous Ulcers?
Arterial ulcers are more painful because oxygen levels are low. The pain can become sharp and strong. Venous ulcers cause dull aching pain that gets better when you raise the leg.
How Do I Know If My Leg Ulcer Is Arterial Or Venous?
You can guess by location and signs. Arterial ulcers sit on the toes or outer legs and feel cold. Venous ulcers sit near the inner ankle with swelling and brown skin. Testing confirms the cause.
Can An Ulcer Be Both Arterial And Venous?
Some ulcers have both arterial and venous causes. These mixed ulcers heal slowly and need both artery and vein care. A clinician uses ABI and duplex testing to find the correct mix.
What Causes Arterial Vs Venous Leg Ulcers To Develop?
Arterial ulcers come from plaque buildup and poor blood flow. Venous ulcers come from valve failure and high pressure in the veins. Both types need early care to prevent harm.
Do Arterial Ulcers Bleed More Than Venous Ulcers?
Venous ulcers may bleed more because they sit in swollen tissue. Arterial ulcers stay dry most time but can bleed if the area is bumped or scraped. Bleeding levels vary from person to person.
Which Ulcer Heals Faster? Venous Or Arterial?
Venous ulcers tend to heal faster when compression is used correctly. Arterial ulcers heal more slowly because the low blood flow must improve before tissue can repair.
How Are Arterial And Venous Ulcers Diagnosed?
Clinicians check pulses, skin signs, and wound appearance. ABI, Doppler, and duplex scans confirm the cause by showing how blood moves through the arteries and veins.
Can Compression Therapy Be Used For Arterial Ulcers?
Compression therapy must not be used for arterial ulcers when arterial flow is low. ABI testing checks safety. Only mild compression is used when the ABI sits in a safe range.
What Are The Best Treatments For Venous Ulcers?
The best treatments include compression, wound dressings, leg elevation, and vein repair when needed. These steps lower pressure and let the skin recover.
How Is An Arterial Ulcer Treated Differently From A Venous Ulcer?
Arterial ulcers need improved blood flow first. Venous ulcers need compression and swelling control. Each plan targets the root problem to help the ulcer heal.
Are Arterial Ulcers Dangerous?
Arterial ulcers can become dangerous because low blood flow starves tissue. Without care, the wound can deepen and risk limb loss. Early testing and treatment reduce this risk.













Leave a Comment