Risk factors for obesity are many. They include social life, culture, medical problems, genes, medicines, stress, and lifestyle habits. Knowing these helps people act before extra weight becomes a health burden. Obesity is not just about eating too much. It is about how the body, the mind, and the environment work together.
Extra body fat affects the endocrine system, raises insulin resistance, and increases chances of cardiovascular conditions and other obesity-related diseases. Each section below explores the real reasons why obesity develops and how they impact daily life.
Social, Cultural, and Economic Risk Factors of Obesity
One strong risk factor of obesity is where people live and work. Areas without parks, gyms, or safe streets limit movement. Stores may lack fresh produce but overflow with packaged meals. Families in such places rely on cheap food high in fat and sugar. Over time, this leads to weight gain and health risks.
Culture shapes food choices too. In some groups, large meals show wealth or care. Social events often involve heavy foods. People may eat more to fit in with their peers. Copying friends and family habits is common. This makes environmental causes of obesity more powerful.
Money plays a major role. Low-income families may skip fresh vegetables and buy processed foods that cost less but pack more calories. High-stress jobs with long shifts also push people toward fast food consumption. These daily patterns create behavioral risk factors for obesity.
Example: A parent working double shifts has no time to cook. They often bring home fried snacks. Children grow up thinking these foods are normal meals. Over time, the whole family faces rising BMI (Body mass index) levels.
Socioeconomic factors such as poor housing, job stress, and lack of health services worsen the issue. The solution requires community effort. More fresh food markets, safe parks, and education campaigns can lower risks.
Genetic Risk Factors for Obesity
Genetic risk factors for obesity explain why some gain weight more easily than others. Over 400 genes may affect appetite, metabolism, fat storage, and hormones. These include genes linked to leptin and ghrelin, hormones that control hunger and fullness.
If both parents have obesity, children face a higher chance of gaining excess weight. However, genes are not destiny. They only set a stage. Lifestyle choices and physical activity still matter.
Rare disorders like Prader-Willi syndrome show extreme genetic influence. Children with it feel constant hunger due to faulty appetite control. More common are small gene changes that increase risk subtly. For example, a gene may slow calorie burning or make fat cells store energy more tightly.
Family history offers clues. If several close relatives live with obesity, early prevention helps. Doctors often monitor children with strong genetic backgrounds closely, guiding diet and movement habits early.
Genes connect with the environment. Someone with genetic risks living in a city with few fresh foods faces higher odds of gaining weight. A person with the same genes but daily outdoor activity may stay healthier. This shows how obesity risk factors build on each other.
Medical Conditions Linked to Obesity
Many medical conditions linked to obesity raise weight in direct and indirect ways. Thyroid disorders slow metabolism. Polycystic ovary syndrome (PCOS) shifts hormonal imbalances, causing fat buildup. Sleep apnea lowers energy and increases appetite. Some chronic conditions like arthritis limit activity levels, leading to lack of physical activity and higher fat storage.
Metabolic disorders such as Cushing’s syndrome raise cortisol levels. High cortisol encourages fat around the belly. This leads to central obesity and more health conditions like high blood sugar.
Another issue is insulin resistance. When cells stop responding well to insulin, blood sugar rises. The body stores extra sugar as fat. This cycle fuels type 2 diabetes and obesity together.
Doctors check for underlying conditions when weight gain is sudden or hard to explain. Treating the root condition can help with weight control. For example, correcting thyroid function often reduces fat storage.
Medication Side Effects That Contribute to Obesity
Some medications cause changes in appetite, hormones, and energy use. Antidepressants like SSRIs can increase cravings. Antipsychotic drugs may raise hunger and lower satiety. Corticosteroids, often used for asthma or arthritis, raise cortisol and shift fat to the abdomen. Certain diabetes drugs store glucose as fat instead of burning it.
Blood pressure medicines such as beta-blockers may lower energy levels, making people less active. Over time, this reduces calorie burning. The result is gradual weight gain.
Patients should never stop their prescribed medications on their own. Instead, they should discuss side effects with their doctor. Often, alternatives exist that have less effect on weight. Doctors may also advise extra activity or diet changes to counteract side effects.
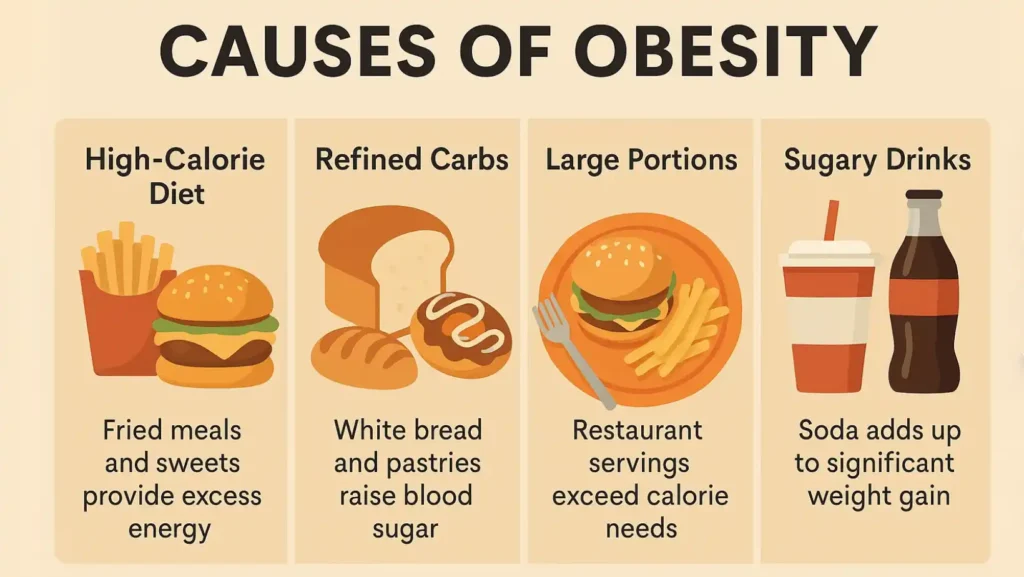
Diet and Nutrition as Causes of Obesity

The most visible causes of obesity are linked to food. A high-calorie diet filled with fried meals, sweets, and sugary drinks packs in more energy than the body can use. Extra calories turn into fat.
Refined carbs like white bread and pastries raise blood sugar quickly. The body releases more insulin, leading to insulin resistance over time. This cycle contributes to obesity-related diseases such as type 2 diabetes.
Another issue is portion size. Restaurant meals often have double or triple the needed calories. Families eating out often may not realize how many extra calories they consume.
Example: A large fast-food combo meal with fries and soda can exceed 1200 calories. That may cover half a day’s needs in one sitting.
People often forget about liquid calories. A single soda adds 150 calories. Two sodas a day equal over 1000 extra calories each week. Over a year, this can mean 10 to 15 pounds of weight gain.
Smart strategies include smaller plates, water instead of soda, and replacing fried snacks with fruits or nuts.
Physical Activity Levels and Sedentary Lifestyle
Low activity is another core driver. A sedentary lifestyle means sitting at a desk, using screens, and rarely moving. This cuts calorie burn and weakens muscles. Without exercise, the body loses balance between energy intake and use.
Children who watch more than 3 hours of TV daily show higher obesity rates. Adults sitting long hours face the same issue. Even regular workouts may not offset long sitting times.
Simple fixes work. Standing up every hour, taking stairs, walking to nearby shops, or cycling to work all add calories burned. Even housework counts as physical activity.
Aiming for 150 minutes of moderate exercise each week helps balance diet and calorie burn. Resistance training builds muscles that keep metabolism higher.
Sleep Quality and Obesity Risk
Sleep and weight connect through hormones. Too little sleep raises ghrelin, which makes people hungrier. At the same time, leptin drops, reducing satiety. This hormone imbalance drives overeating. Short nights also raise cortisol, pushing fat storage around the belly.
Studies show that adults sleeping under 6 hours a night are more likely to gain weight. Children with irregular bedtimes also face higher risks. Poor or broken sleep means poor sleep patterns, which lower energy for activity the next day.
Improving sleep by setting a routine, keeping screens away before bedtime, and managing sleep apnea can lower obesity risk.
Stress Levels and Behavioral Risk Factors
Stress shapes eating patterns in unhealthy ways. High tension often pushes people to snack or binge. This emotional eating provides short relief but adds excess calories. Stress also cuts time and energy for cooking or physical activity.
The hormone cortisol rises with stress. This leads to more abdominal fat. The body treats stress as a signal to store energy. Chronic stress also disrupts sleep, raising obesity risk further.
Examples of behavioral risk factors obesity include skipping meals, fast eating, and late-night snacks. Each of these increases calorie intake and changes metabolism.
Stress management through relaxation, breathing exercises, and social support reduces the urge to overeat.
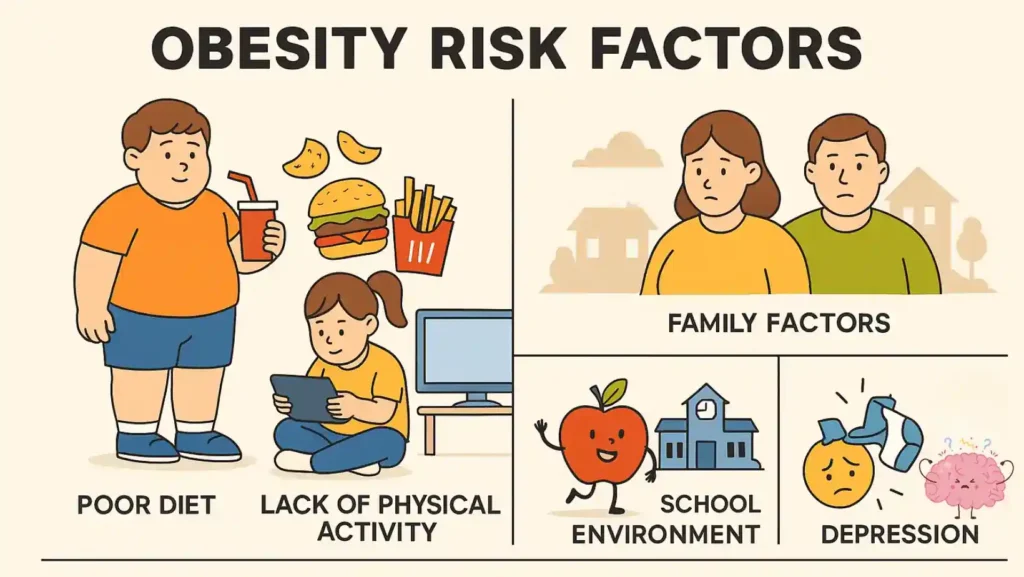
Childhood Obesity: Risk Factors, Health Effects, and Prevention
Children face unique risks. Childhood obesity risk factors, health effects and prevention must be studied together. Kids often eat more processed snacks, sugary drinks, and larger portions. They also spend more hours on screens and less time in outdoor play.
Family patterns are key. Parents with obesity often pass both genes and eating habits to kids. Unsafe neighborhoods limit play. Schools with few physical education classes reduce activity. These factors add up quickly.
The health effects of childhood obesity include early type 2 diabetes, asthma, joint pain, and even depression. Children with obesity often face bullying, which worsens stress and emotional eating.
Prevention works best when started early. Families can offer healthy meals, water instead of soda, and encourage outdoor play. Schools can provide daily physical activity and nutrition lessons. Governments can reduce sugary drink sales near schools.
Doctors advise parents to watch growth charts closely. Small changes in childhood often prevent serious problems in adulthood.
The Bottom Line
Obesity risk factors come from many sides. Genes, environment, stress, food, sleep, and medical care all play roles. Each factor alone may not cause obesity, but together they create strong risk.
The good news is that small actions cut risk. Families can focus on better food, more play, less screen time, and good sleep. Adults can manage stress, move more, and talk with doctors about medicines and conditions. Communities and governments must also help by making healthy choices affordable and safe.
Obesity is not a single problem with one solution. There are many small issues joined together. The more we understand, the better we can act.
FAQs
What are the main risk factors for obesity?
They include poor diet, lack of activity, poor sleep, stress, medicines, genes, and related health conditions that increase fat storage.
What are 5 risks of obesity?
Obesity increases the chance of type 2 diabetes, high blood pressure, cardiovascular conditions, joint pain, and some cancers due to fat buildup.
What are the risk factors for central obesity?
Central obesity risks include stress, high sugar diet, aging, hormonal imbalances, and insulin resistance, which increase belly fat storage.
What are the 4 causes of obesity?
The four main causes are excess calories, low physical activity, genetic influence, and effects from certain medications or medical disorders.
What are the 4 types of obesity?
Types include central abdominal obesity, peripheral obesity, obesity from endocrine system issues, and genetic-related obesity seen early in life.
What organ is most affected by obesity?
The heart suffers most, as obesity increases cardiovascular conditions. The liver also develops fatty changes that harm long-term health.
What are the risk factors for obesity in children?
Child risks include high sugar intake, screen time, little play, poor sleep, and family lifestyle habits that reduce healthy activity.













Leave a Comment