Side effects of obesity surgery are a subject that every patient must understand before taking a decision. Surgery offers dramatic weight loss, but it comes with short-term and long-term changes in health. People often assume the surgery itself is the cure, but the truth is that surgery is only a tool. Lifestyle adjustments, nutritional care, and medical follow-up are required for life. If ignored, serious harm may occur.
This article explains in detail the types of obesity surgery, their complications, the medical science behind them, and the daily-life impact patients face after surgery. You will find in-depth analysis, clear examples, and practical insights not found in standard guides.
Gastric Sleeve Surgery: Side Effects and Risks
The gastric sleeve, also called sleeve gastrectomy, is one of the most performed weight loss surgeries. In this procedure, about 70–80% of the stomach is permanently removed. What remains is a narrow, tube-like stomach. The reduced size lowers food intake and removes most of the stomach’s hunger-producing hormone ghrelin, which decreases appetite.
But the benefits come with clear risks of gastric sleeve surgery.
Short-term side effects include:
- Nausea and vomiting as the digestive system adapts.
- Abdominal pain, gas, and bloating from surgery trauma.
- Acid reflux or worsening of pre-existing reflux.
- Stenosis, which is narrowing of the stomach sleeve, leading to difficulty swallowing.
Serious risks:
- Staple line leaks are the most feared complication. If stomach fluids leak into the abdominal cavity, infection and sepsis can occur.
- Bowel perforation though rare, can be life-threatening.
- Bleeding requiring transfusion or reoperation.
Long-term consequences:
- Nutrient deficiencies after obesity surgery are common. Patients lose Iron, B12, and Calcium. Without supplementation, this can lead to anemia, weak bones, and osteoporosis.
- Some patients develop food intolerance for meat, dairy, or high-fiber foods.
- Chronic constipation or diarrhea depending on dietary choices.
Example: A 45-year-old patient who lost 120 pounds after sleeve surgery developed severe heartburn, needing daily medication. Later, due to poor supplement intake, she developed low Calcium levels, leading to bone fractures.
This case highlights that weight loss is not the end of the journey. The risks remain and must be monitored for life.
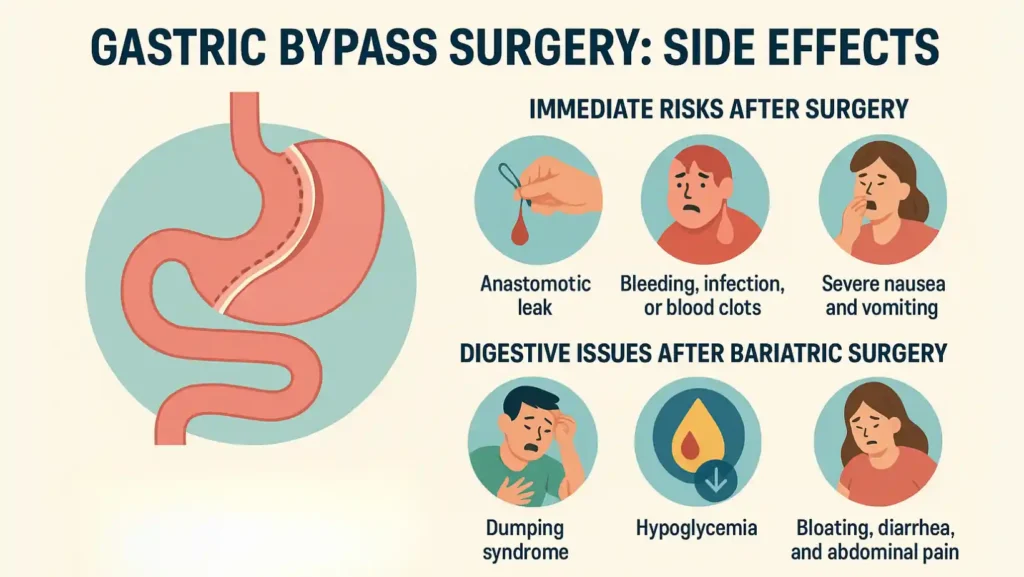
Gastric Bypass Surgery: Side Effects and Complications
Gastric bypass is more complex. It creates a small pouch from the stomach and connects it directly to the small intestine. This reduces food intake and also limits absorption. The result is rapid, dramatic weight loss. However, it is also linked with notable gastric bypass side effects.
Immediate risks after surgery:
- Anastomotic leak at the surgical join between stomach and intestine.
- Bleeding, infection, or blood clots.
- Severe nausea and vomiting in the first weeks.
Digestive issues after bariatric surgery:
- Dumping syndrome is very common. Patients feel dizzy, sweaty, and weak after eating sugary food. This happens because the stomach pouch empties too fast into the small intestine.
- Hypoglycemia (low blood sugar) can develop hours after eating, especially in people sensitive to insulin spikes.
- Bloating, diarrhea, and abdominal pain are frequent when patients eat fatty or fried food.
Nutritional effects:
Because absorption is reduced, patients face vitamin deficiency and malnutrition if they skip supplements. Iron deficiency leads to fatigue and weakness. Lack of Calcium causes fragile bones. Vitamin B12 deficiency may cause nerve damage.
Other long-term complications:
- Gallstones after surgery form quickly because of rapid weight loss.
- Stenosis at the surgical connection may block food flow, causing constant vomiting.
- Risk of bowel obstruction and internal hernia.
Example: A 32-year-old woman lost 100 pounds in one year after bypass. However, she started fainting due to hypoglycemia. She later required special diet counseling to balance sugar intake.
This shows bypass is powerful but requires strict diet control and supplements. Patients must accept that lifelong follow-up is essential.
Adjustable Gastric Band Surgery: Risks and Side Effects
Adjustable gastric banding places a silicone band around the upper stomach. The band can be inflated or deflated with saline to control restriction. It was once popular, but over the years, it has lost favor because of high complication rates.
Post-bariatric surgery side effects specific to the band include:
- Band slippage where the band moves from its place, causing pain and vomiting.
- Outlet obstruction blocking food passage.
- Esophageal dilation when the food pipe enlarges because of chronic pressure.
- Nausea, vomiting, and acid reflux are common when the band is too tight.
Device-related risks:
- Band leakage or infection.
- In some cases, the band erodes into the stomach wall.
- Many patients require revision or removal within 5–10 years.
Although the surgery avoids cutting or rerouting the stomach, its complications make it less effective compared to sleeve or bypass.
Biliopancreatic Diversion With Duodenal Switch (BPD-DS): Complications and Long-Term Effects
BPD-DS is the most powerful and complex form of bariatric surgery. It involves removing part of the stomach (like a sleeve) and rerouting the intestine (like a bypass). It results in extreme calorie malabsorption.
Short-term side effects:
- Diarrhea and foul-smelling stools due to fat malabsorption.
- Nausea & vomiting, and abdominal pain during the adjustment period.
- Bowel perforation and leaks as with other surgeries.
Long-term side effects:
- Severe nutrient deficiencies after obesity surgery are highest in this group. Patients lose protein, fat-soluble vitamins (A, D, E, K), and minerals.
- Iron and Calcium loss are significant, with risk of osteoporosis and bone fractures.
- Food intolerance is common, with many avoiding fatty and dairy-rich foods.
- Malnutrition is a serious threat if supplements are not taken daily.
While weight loss is greatest, this operation requires the most disciplined follow-up.
Example: A 50-year-old man who underwent BPD-DS achieved massive weight loss, reversing his diabetes. However, he developed severe vitamin A deficiency, leading to vision problems, as he missed supplement checks.
This proves that strong results also bring strong risks.
General Bariatric Surgery Complications To Know
Across all types of obesity surgery, there are shared problems. These include:
- Weight loss surgery risks like infection, clots, and poor wound healing.
- Digestive issues after bariatric surgery including constipation, diarrhea, or bloating.
- Loose skin after weight loss surgery due to rapid fat loss, often requiring cosmetic surgery.
- Gallstones after surgery as the liver processes fat too quickly.
- Dumping syndrome especially in bypass patients.
- Vitamin deficiency leading to anemia, nerve issues, and weak bones.
- Rare events like anastomotic leak, bowel perforation, and chronic abdominal pain.
A clear comparison of surgeries helps patients see the balance between risks and benefits.
| Surgery Type | Weight Loss Effect | Main Side Effects | Long-Term Risks | Nutrient Risk Level |
| Gastric Sleeve | 60–70% of excess | Acid reflux, nausea, stenosis | Bone loss, food intolerance | Medium |
| Gastric Bypass | 65–80% of excess | Dumping, hypoglycemia, diarrhea | Gallstones, bowel obstruction | High |
| Gastric Band | 40–50% of excess | Band slippage, reflux, vomiting | Device erosion, esophageal dilation | Low–Medium |
| BPD-DS | 70–85% of excess | Diarrhea, foul stools | Severe malnutrition, osteoporosis | Very High |
The Bottom Line
The choice is never between “safe” and “unsafe.” It is about choosing the surgery that balances weight loss benefits with possible bariatric surgery complications. Patients must compare the long-term effects of obesity with the possible side effects of surgery.
Untreated obesity raises the risk of diabetes, heart disease, stroke, and cancer. These conditions shorten life. Surgery lowers those risks but creates new health needs. Every patient must commit to regular checkups, lifelong vitamins, and dietary care.
The bottom line is simple: Surgery works, but only when paired with discipline and long-term medical guidance.
FAQs
Are there any long-term side effects from bariatric surgery?
Yes. Nutrient deficiencies, diarrhea, reflux, and bone loss are long-term side effects. Careful monitoring and supplementation reduce these risks significantly.
Is obesity surgery safe?
Modern obesity surgery is safer than before. However, leaks, infections, and deficiencies remain risks. Safety depends on patient commitment and the surgeon’s skill.
What are the risks of surgery for obese patients?
Risks include bleeding, infection, clots, and leaks. Long-term, patients may face malnutrition, bowel obstruction, or gallstones. Regular care lowers these risks.
What are the risks of long term obesity?
Long-term obesity causes diabetes, heart disease, liver disease, sleep apnea, and some cancers. It reduces lifespan and quality of life significantly.
What is the safest weight loss surgery?
Safety depends on the patient. Sleeve and bypass are common choices. Gastric band is less invasive but less effective. Each option has unique risks.
What lifestyle changes are needed after surgery?
Smaller meals, no sugary foods, lifelong vitamins, exercise, and medical follow-ups are needed. Without these changes, health risks and complications increase.
What is the recovery time for weight loss surgery?
Most patients recover in 2–6 weeks. Hospital stay is 2–3 days. Heavy work and intense activity may need 6–8 weeks of rest.












Leave a Comment