Medically reviewed by Dr Chandril Chugh,
Renowned Neurologist and American Trained Specialist
Welcome to an enlightening journey through the world of prostate cancer treatments. Prostate cancer is the second most frequent disease globally, with an estimated 1.4 million new cases reported in 2020. As the incidence of prostate cancer continues to rise, it becomes crucial to explore the development and implementation of the best treatments for this condition. In this article, we will delve into the advancements in prostate cancer treatments, with a special focus on nanotherapeutics in the Gulf countries.
Table of Contents
ToggleKey Takeaways:
- Prostate cancer is the second most frequent disease worldwide.
- The incidence of prostate cancer is higher in Gulf countries.
- Nanotherapeutics offer exciting possibilities for prostate cancer treatment.
- Understanding prostate cancer and its risk factors is crucial for effective treatment.
- Stay informed about the latest advancements in prostate cancer treatment.
Understanding Prostate Cancer
Prostate cancer is the most common type of cancer affecting modern-day men after lung cancer. It primarily affects men in the age group of 66 years and above. The incidence of prostate cancer is higher in regions with a high human development index, including Gulf countries. Common risk factors for prostate cancer include age, family history, and unhealthy lifestyle habits such as obesity and tobacco and alcohol consumption.
It is essential to understand the key risk factors associated with prostate cancer. Age is a major factor, as the incidence of prostate cancer increases with advancing age. Family history also plays a role, with men who have close relatives diagnosed with prostate cancer being at higher risk. Unhealthy lifestyle habits, such as a sedentary lifestyle, obesity, and tobacco and alcohol consumption, have also been linked to an increased risk of developing prostate cancer.
In Gulf countries, the incidence of prostate cancer is relatively high due to various factors, including improved access to healthcare and longer life expectancies. The Gulf region has witnessed significant economic growth and development, leading to an increase in the prevalence of lifestyle diseases, including prostate cancer.
A study conducted in Gulf countries found that the average age of prostate cancer diagnosis is 68 years, with a higher incidence in older age groups. This highlights the importance of regular screenings and awareness among older individuals to detect prostate cancer at an early stage when treatment options are more effective.
Prostate cancer is a complex disease influenced by various factors. By understanding the risk factors and taking proactive steps towards prevention, including a healthy lifestyle and regular screenings, you can reduce the risk of prostate cancer and improve your overall well-being.
Let’s take a look at a comprehensive table summarizing the risk factors associated with prostate cancer:
| Risk Factors | Description |
|---|---|
| Age | The risk of prostate cancer increases with advancing age, primarily affecting men above 66 years old. |
| Family History | Men with close relatives diagnosed with prostate cancer have an increased risk. |
| Lifestyle Habits | Unhealthy lifestyle habits such as obesity, sedentary lifestyle, tobacco, and alcohol consumption can contribute to a higher risk of prostate cancer. |
Remember, maintaining a healthy lifestyle and staying proactive with regular screenings are crucial in managing the risk of prostate cancer.
Stay Informed, Stay Healthy
Regular screenings, healthy lifestyle choices, and increased awareness can go a long way in preventing and managing prostate cancer. By understanding the risk factors and taking necessary precautions, you can prioritize your health and well-being. In the next section, we will delve into the global incidence of prostate cancer, providing insights into the scale of this disease on a global level.
Global Incidence of Prostate Cancer
Prostate cancer is a significant global health issue, affecting men worldwide. In 2020 alone, there were an estimated 1.4 million new cases of prostate cancer reported globally. The incidence of prostate cancer varies across different regions, with Europe and Asia experiencing the highest number of new cases. It is crucial to understand the global statistics of prostate cancer to develop effective treatment strategies and address this widespread health concern.
Regional Variation in Incidence
The incidence rates of prostate cancer differ across regions, reflecting variations in risk factors, healthcare access, and screening practices. Europe and Asia have consistently reported high numbers of new prostate cancer cases, contributing significantly to the global incidence. In contrast, regions such as Africa, Europe, and North America have higher mortality rates associated with prostate cancer, emphasizing the importance of early detection and comprehensive treatment options.
Mortality Rates
Prostate cancer is the fifth leading cause of cancer-related deaths in men worldwide. The highest mortality rates are observed in Africa, Europe, and North America, reflecting the challenges faced in managing advanced stages of the disease. Improved access to healthcare, timely screenings, and advancements in treatment modalities are crucial to reducing the mortality rates associated with prostate cancer globally.

Why Global Prostate Cancer Statistics Matter
Understanding the global incidence of prostate cancer is vital in shaping public health policies, allocating resources, and implementing effective prevention and treatment strategies. By analyzing global statistics, healthcare professionals and policymakers can identify high-risk regions, plan targeted screenings, and develop region-specific interventions to improve patient outcomes.
Furthermore, global statistics help researchers identify trends, risk factors, and potential areas for targeted research and innovation. Collaborative efforts across countries and regions can enable the exchange of knowledge, best practices, and advancements in prostate cancer management, ultimately benefiting patients worldwide.
Prostate Cancer in Gulf Countries
Gulf countries, including Saudi Arabia, have witnessed a gradual increase in the incidence of prostate cancer over the past decade. In 2020, the age-standardized incidence rate (ASIR) for prostate cancer in Saudi Arabia was 7 per 100,000 men, with an age-standardized mortality rate (ASMR) of 2.5 per 100,000 men. It is noteworthy that the age-standardized rate of prostate cancer in Arab countries is relatively lower compared to Europe and North America, which can be attributed to factors such as limited PSA test screening and specific biological differences among Arab men.

Prostate Cancer Incidence and Mortality Rates in Gulf Countries
| Country | Incidence Rate (per 100,000 men) | Mortality Rate (per 100,000 men) |
|---|---|---|
| Saudi Arabia | 7 | 2.5 |
| United Arab Emirates | 6.5 | 2.2 |
| Kuwait | 6 | 2 |
| Qatar | 5.8 | 2.1 |
The data above highlights the incidence and mortality rates of prostate cancer in Gulf countries, indicating the significant health burden posed by this disease. These statistics reflect the importance of raising awareness about prostate cancer and implementing effective screening and treatment strategies to combat its impact on men’s health in the Gulf region.
Prostate Cancer Screening Controversy
Prostate cancer screening has sparked debates and controversies in the medical community, particularly regarding the use of the prostate-specific antigen (PSA) test. Many experts question the effectiveness of screening and its ability to reduce the risk of death from prostate cancer.
The PSA test, which measures the level of prostate-specific antigen in the blood, has shown conflicting results in studies. While it can detect prostate cancer at an early stage, there is no clear evidence that screening with the PSA test improves survival rates. Systematic reviews and meta-analyses have failed to demonstrate significant benefits of screening, raising concerns about the potential harms.
One of the main concerns is the issue of overdiagnosis and overtreatment. PSA testing has led to the identification of clinically indolent tumors, which are slow-growing and may not cause any harm if left untreated. However, once diagnosed, patients often undergo aggressive treatments such as surgery, radiation therapy, or hormone therapy, which can have significant side effects and impact the quality of life.
Experts argue that the benefits of screening must outweigh the potential harms for it to be recommended as a routine practice. This necessitates a thorough evaluation of each individual’s risk factors, age, and overall health status to determine the appropriateness of prostate cancer screening. Shared decision-making between patients and healthcare providers is crucial in making informed choices about screening.
In conclusion, the controversy surrounding prostate cancer screening and the PSA test highlights the need for further research and a more nuanced approach to cancer detection. While early detection is crucial, it is essential to consider the potential benefits and harms of screening in individual cases to make informed decisions about prostate cancer management.

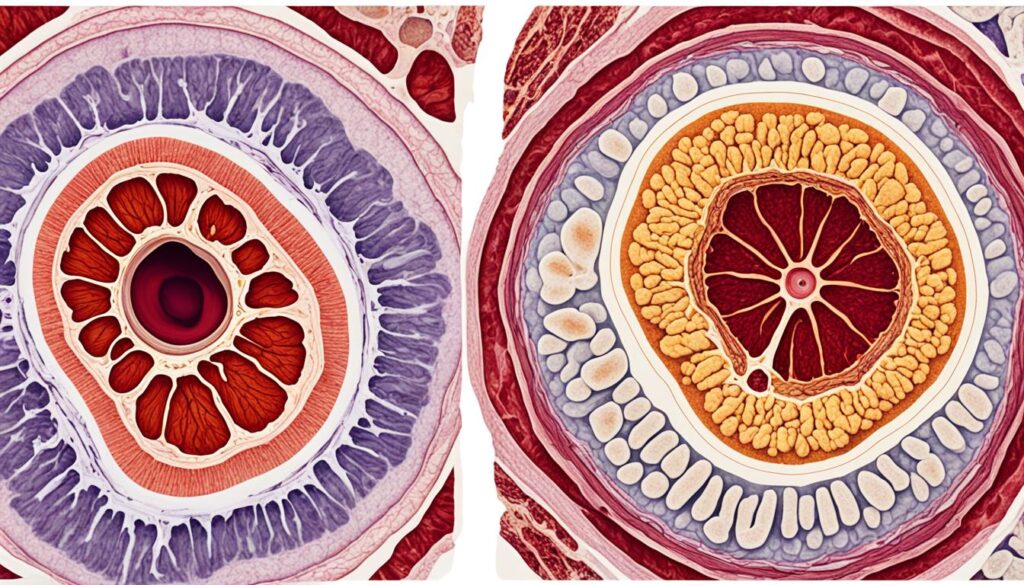
Diagnostic Evaluation of Prostate Cancer
When it comes to diagnosing prostate cancer, needle biopsy is the most common method used by urologists. This procedure involves using a bioptic gun with ultrasound guidance to collect tissue samples from the prostate for further examination.
Another diagnostic tool that is gaining attention is magnetic resonance imaging (MRI)-directed biopsy. This technique allows for more targeted sampling of suspicious areas identified on the MRI scan, potentially improving the accuracy of the diagnosis.
During the diagnostic evaluation of prostate cancer, several factors are taken into consideration. One important factor is the histological grade of the tumor, which is assessed using the Gleason scoring system. This scoring system helps determine the aggressiveness of the cancer and guide treatment decisions.
Additionally, the prostate-specific antigen (PSA) level in the blood is an important factor in diagnosing prostate cancer. Elevated PSA levels may indicate the presence of cancer and can help guide further diagnostic procedures and treatment plans.
Diagnostic Evaluation Methods for Prostate Cancer
| Diagnostic Method | Description |
|---|---|
| Needle Biopsy | A common method that involves collecting tissue samples from the prostate using a bioptic gun with ultrasound guidance. |
| MRI-Directed Biopsy | A technique that allows for more targeted sampling of suspicious areas identified on an MRI scan, potentially improving diagnostic accuracy. |
| Gleason Scoring System | A system used to assess the histological grade of prostate tumors and determine the aggressiveness of the cancer. |
| PSA Level | The measurement of prostate-specific antigen in the blood, which can indicate the presence of prostate cancer. |
These diagnostic evaluation methods play a crucial role in accurately diagnosing prostate cancer and guiding treatment decisions. It’s important for healthcare professionals to consider multiple factors, including histological grading, PSA levels, and imaging techniques, to ensure an accurate diagnosis and personalized treatment plan for each patient.
Optimal Treatment Approaches for Prostate Cancer
Treatment approaches for prostate cancer depend on various factors, including the stage and grade of the tumor, your age and overall health, and your preferences as well as the recommendation of your healthcare provider.
There are several options available for prostate cancer treatment:
- Surgery: One of the optimal approaches is surgery, specifically radical prostatectomy, which aims to remove the prostate gland and nearby tissues. This can be done through open surgery or minimally invasive techniques such as laparoscopic or robotic-assisted surgery.
- Radiation therapy: Another effective approach is radiation therapy, which uses high-energy beams to kill cancer cells. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy) depending on the specific situation and recommendation of your healthcare provider.
- Hormone therapy: Hormone therapy aims to reduce the levels of male hormones, like testosterone, that help prostate cancer grow. It can be achieved through medications that block the production or action of these hormones.
- Active surveillance: For some patients with low-risk prostate cancer, active surveillance may be a viable option. This involves careful monitoring of the disease using periodic PSA tests, digital rectal exams, and imaging studies. Treatment is delayed until there is evidence of disease progression.
It is important to discuss these treatment options with your healthcare provider to determine the best approach based on your individual circumstances. The decision-making process should take into consideration the potential benefits, risks, and side effects of each treatment option.
Advances in Nanotherapeutics for Prostate Cancer
Nanotherapeutics, a field that combines nanotechnology and therapeutics, holds tremendous promise for the treatment of prostate cancer. By utilizing nanoparticles, targeted therapy can be delivered directly to cancer cells, improving treatment efficacy while minimizing side effects. Moreover, nanotherapeutics can revolutionize drug delivery, enhancing the bioavailability of therapeutic agents and optimizing their effectiveness.
Over the years, several studies have showcased promising results in the development and implementation of nanotherapeutics for prostate cancer treatment, particularly in Gulf countries. These advancements offer new hope for patients and healthcare professionals in the fight against this prevalent disease.
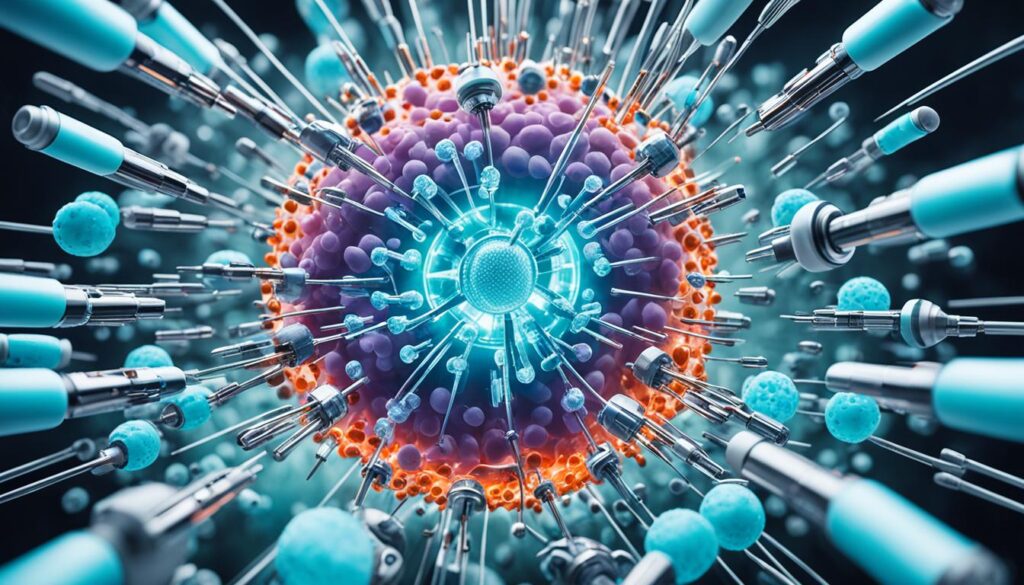
One of the key advantages of nanotherapeutics is their ability to precisely deliver drugs to tumor sites. By targeting specific cancer cells, these nanoscale drug carriers can effectively increase treatment efficacy while reducing damage to healthy tissues. This targeted therapy approach allows for higher drug concentrations at the desired site, enhancing the chances of eliminating cancer cells and improving patient outcomes.
Besides targeted therapy, nanotherapeutics also play a significant role in drug delivery optimization. The use of nanoparticles allows for controlled and sustained release of therapeutic agents, providing a steady supply of medication to the tumor site. This sustained drug delivery not only maximizes treatment effectiveness but also minimizes unwanted side effects, leading to improved patient comfort and quality of life.
The field of nanotherapeutics continues to evolve, with ongoing research and development efforts focused on refining and expanding their applications in prostate cancer treatment. With further advancements, nanotherapeutics hold the potential to revolutionize the landscape of cancer therapy, providing more personalized and effective treatment options for prostate cancer patients.
Long-Term Results with TULSA Ablation
TULSA (transurethral ultrasound ablation) offers a minimally invasive treatment option for localized prostate cancer. This innovative approach has shown promising long-term outcomes in terms of disease control and patient outcomes.
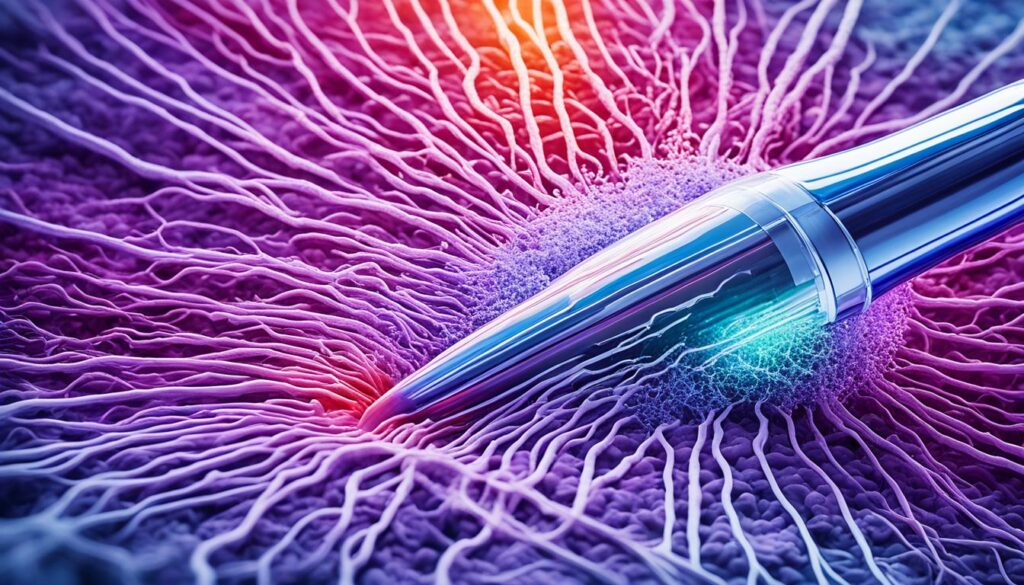
Recent studies have demonstrated the effectiveness of TULSA ablation in providing lasting disease control. The TACT trial, a landmark study, reported impressive results after five years of follow-up. The trial revealed that whole-gland TULSA ablation achieved durable disease control with a low rate of salvage treatments.
TULSA ablation shows particular promise for patients with intermediate-grade focal or regional tumors that are not adjacent to the urethra or prostate apex. By targeting specific areas of the prostate, this innovative treatment option allows for precise and effective disease control.
Additionally, TULSA ablation offers a favorable toxicity profile, minimizing the risk of complications and side effects. This makes it an attractive treatment option for patients seeking optimal outcomes with a reduced risk of adverse events.
In summary, the long-term results of TULSA ablation demonstrate its effectiveness in localized prostate cancer treatment. The ability to achieve disease control and reduce the need for salvage treatments makes it a promising approach. Consult with your healthcare provider to evaluate if TULSA ablation is a suitable treatment option for you.
Radiopharmaceutical Therapy for Metastatic Prostate Cancer
Radiopharmaceutical therapy is a promising treatment approach for metastatic castration-resistant prostate cancer (mCRPC). Specifically, the use of the radiopharmaceutical 225Ac-J591 has shown encouraging results in clinical trials.
The radiopharmaceutical 225Ac-J591 consists of a monoclonal antibody that is radiolabeled with the alpha emitter actinium-225. This targeted therapy aims to deliver radiation directly to cancer cells, minimizing damage to healthy tissues.
In phase 1 trials, 225Ac-J591 has demonstrated the ability to produce responses across metastatic sites. Notably, higher response rates have been observed in visceral and bone lesions compared to lymph nodes.
Further research is needed to determine the optimal use of targeted radionuclide therapies like 225Ac-J591 in the treatment of mCRPC. However, the initial findings suggest that radiopharmaceutical therapy holds great promise as a potential option for patients with advanced metastatic prostate cancer.
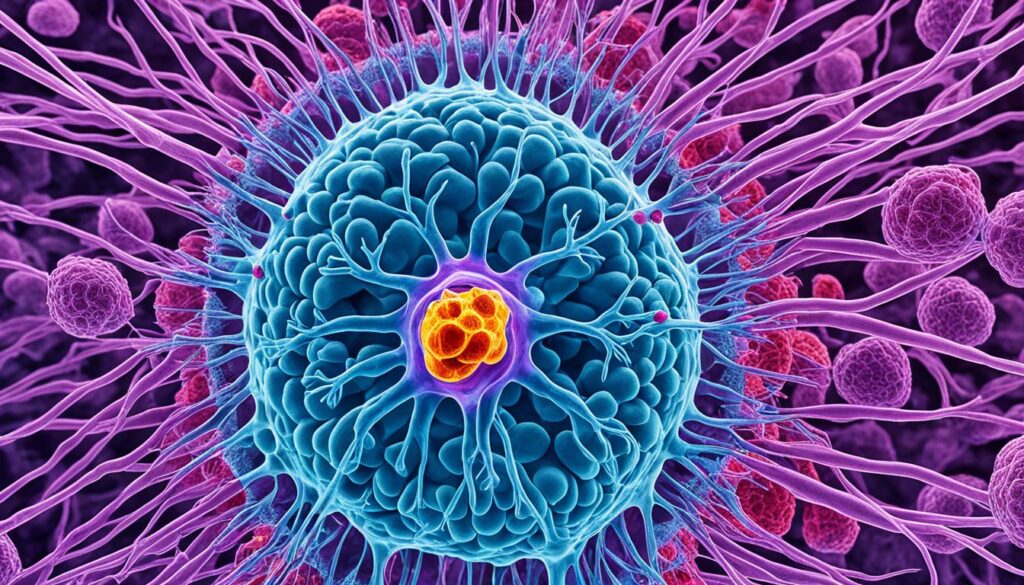
Further research is needed to determine the optimal use of targeted radionuclide therapies in the management of metastatic castration-resistant prostate cancer. Nevertheless, 225Ac-J591 shows promising potential as a novel treatment modality for patients with advanced prostate cancer.
Integrating Genomic and Clinicopathologic Risk in Prostate Cancer
Integrating genomic and clinicopathologic risk information can play a crucial role in enhancing risk stratification and prognostication in prostate cancer. Numerous studies have demonstrated significant variations in genomic risk among a large cohort of prostate cancer patients. Combining genomic and clinicopathologic risk categories has the potential to result in improved outcomes. Through the integration of these factors, stage reclassifications become possible, leading to more accurate risk assessment.
By combining genomic and clinicopathologic information, healthcare professionals can better identify patients who may require more aggressive treatment approaches. This integrated approach aids in the informed decision-making process, enabling personalized treatment plans that are tailored to individual patient needs. Understanding both the genomic and clinicopathologic aspects of prostate cancer provides a comprehensive foundation for developing effective treatment strategies.
Genomic risk assessment involves the analysis of an individual’s genetic profile to identify specific genetic alterations that may contribute to the development and progression of prostate cancer. Clinicopathologic risk evaluation, on the other hand, takes into account various clinical factors such as tumor stage, grade, and other pathologic characteristics, along with demographic and clinical information.
As the field of genomics continues to advance, the integration of genomic and clinicopathologic risk information is becoming increasingly valuable in precision medicine. This integrated approach holds great promise for optimizing risk stratification, prognostication, and treatment decisions in prostate cancer.
Understanding the genomic and clinicopathologic aspects of prostate cancer and their integration is crucial for both patients and healthcare professionals. Effective risk stratification and prognostication can empower patients to make informed decisions about their treatment options. By combining genomic and clinicopathologic risk information, healthcare professionals can provide personalized care plans that maximize the potential for positive outcomes.
Conclusion
Prostate cancer remains a significant health concern worldwide, with a high incidence and mortality rate. When it comes to choosing the best treatment for prostate cancer, several factors must be considered. These include the stage and grade of the tumor, the patient’s age and overall health, and individual preferences.
Fortunately, advancements in the field of prostate cancer treatment offer promising options. Nanotherapeutics, such as targeted therapy using nanoparticles, show potential for delivering optimal treatments directly to cancer cells while minimizing side effects. TULSA ablation, a minimally invasive treatment, has demonstrated long-term disease control for localized prostate cancer.
Radiopharmaceutical therapy, using substances like 225Ac-J591, has shown promise in treating metastatic castration-resistant prostate cancer. By combining genomic and clinicopathologic risk factors, healthcare professionals can better stratify patients and make more informed treatment decisions.
As research continues to advance, ongoing efforts to improve the prognosis and quality of life for prostate cancer patients remain a top priority. By staying up-to-date with the latest advancements and working closely with healthcare providers, individuals can navigate the complex landscape of prostate cancer treatments and find the optimal approach for their unique situation.
FAQ
What are the best treatments for prostate cancer?
The optimal treatment approaches for prostate cancer depend on various factors, including the stage and grade of the tumor, the patient’s age and overall health, and individual preferences. Options may include surgery, radiation therapy, hormone therapy, and active surveillance.
What are the risk factors for prostate cancer?
The most common risk factor for prostate cancer is age, with men in the age group of 66 years and above being the most vulnerable. Other risk factors include family history, unhealthy lifestyle habits such as obesity, and tobacco and alcohol consumption.
How common is prostate cancer globally?
Prostate cancer is the second most frequent disease in the world, with an estimated 1.4 million new cases reported worldwide in 2020. It is the fifth leading cause of male cancer-related deaths globally.
Is the incidence of prostate cancer higher in Gulf countries?
Yes, the incidence of prostate cancer is higher in regions with a high human development index, including Gulf countries. In Saudi Arabia, the age-standardized incidence rate (ASIR) for prostate cancer was 7 per 100,000 men in 2020.
What are the controversies surrounding prostate cancer screening?
Prostate cancer screening, particularly through the use of the prostate-specific antigen (PSA) test, remains controversial. There is conflicting evidence regarding whether screening decreases the risk of death from prostate cancer, and the potential harms of overdiagnosis and overtreatment have been observed.
How is prostate cancer diagnosed?
The most common method used to diagnose prostate cancer is a needle biopsy. Urologists may perform a transrectal biopsy using a bioptic gun with ultrasound guidance. Magnetic resonance imaging (MRI)-directed biopsy is also being studied as an alternative or additional diagnostic tool. The diagnosis is based on factors such as the histological grade of the tumor, assessed using the Gleason scoring system, and the prostate-specific antigen (PSA) level in the blood.
What are the advances in nanotherapeutics for prostate cancer?
Nanotherapeutics, which combine nanotechnology and therapeutics, show promise for the treatment of prostate cancer. Nanoparticles can be engineered to deliver targeted therapy directly to cancer cells, improving treatment efficacy and reducing side effects. They can also enhance drug delivery and improve the bioavailability of therapeutic agents.
What is TULSA ablation for prostate cancer?
TULSA (transurethral ultrasound ablation) is a minimally invasive treatment option for localized prostate cancer. Recent studies have shown that TULSA can provide long-term disease control with a favorable toxicity profile. It may be suitable for patients with intermediate-grade focal or regional tumors that are not adjacent to the urethra or prostate apex.
What is radiopharmaceutical therapy for metastatic prostate cancer?
Radiopharmaceutical therapy, specifically using the radiopharmaceutical 225Ac-J591, has shown promise for the treatment of metastatic castration-resistant prostate cancer (mCRPC). It consists of a monoclonal antibody radiolabeled with the alpha emitter actinium-225. Phase 1 trials have shown positive responses across metastatic sites, with higher response rates observed in visceral and bone lesions.
How can genomic and clinicopathologic risk information help in prostate cancer?
Integrating genomic and clinicopathologic risk information may improve risk stratification and prognostication in prostate cancer. Studies have shown wide variation in genomic risk across a large cohort of patients, suggesting that combining genomic and clinicopathologic factors can lead to better outcomes and more accurate risk assessment.
